
This post was written by Jennifer Rechter, MSN, RN-BC, AG-CNS, clinical nurse specialist of MICU and 3 South, sepsis coordinator, Parkview Health.
Sepsis is considered a global health care problem that takes more lives than cancer and occurs more frequently than heart attacks [1]. Because of this risk, Parkview Health is constantly working to minimize the risk for patients and educate the public about this frightening condition.
September has been named National Sepsis Awareness Month by the Sepsis Alliance. The goal is to increase knowledge and awareness of sepsis, not just for those in the medical field but also to families, patients and communities. This is particularly important, as around 87% of sepsis cases are acquired outside the hospital, making it a public health issue, not just a condition the hospital needs to address. [1]
To aid in this goal, the Sepsis Alliance asks that we all come together to support the effort and save lives by promoting sepsis awareness. We can all do our part by sharing and broadcasting the sepsis message of “See it. Stop it. Survive it.” This message focuses on the importance of being able to recognize symptoms and seek treatment quickly, just like we do for heart attacks and strokes. [1]
What is sepsis?
Sepsis is the body’s overwhelming and potentially life-threatening response to an infection, which can lead to tissue damage, organ failure and even death. [1]
Who is at risk for sepsis?
Sepsis can affect anyone, but according to the Centers for Disease Control and Prevention (CDC), some populations are at a higher risk. [2] Specifically, those who:

What causes sepsis?
Any infection can lead to sepsis. Here are the four most common infections associated with sepsis:

What are the signs or symptoms of sepsis?
Unfortunately, there is no single sign or symptom because sepsis can occur from any infection. With that said, diarrhea, vomiting and a sore throat are the most common indications of an infection. Additionally, those suffering from sepsis might also experience the following [1]:
Shivering, fever, feeling very cold
Extreme pain or feeling worse than ever
Pale or discolored skin
Sleepiness, difficulty waking up, confusion
I feel like I might die
Shortness of breath
If you have any of the above symptoms in addition to an infection, you should seek medical care immediately.
Act fast when it comes to sepsis:
Acting fast and seeking prompt medical care is critical when sepsis is suspected, along with being aware of the signs and symptoms of sepsis [1].
How can I prevent sepsis?
Sadly, there is no single way to prevent sepsis, but there are many things you can do to reduce your risk of developing sepsis. [1]
- Get vaccinated: Flu, pneumonia, COVID and other infections can lead to sepsis, so it’s very important you protect yourself. Talk to your healthcare provider for more information on vaccinations.
- Be thorough: Practice good hygiene. Practice proper handwashing, brush your teeth and bathe regularly. If you have scrapes or wounds, clean them properly and follow treatment recommendations. If you notice any delays in healing seek medical care.
- Be vigilant: Be aware of any signs like fever, chills, increased breathing and heart rate, confusion, and disorientation if you have an infection.
What is Parkview doing to identify sepsis early?
In January of 2019, the Sepsis Task Force team, in collaboration with the Business Intelligence-Analytic team, implemented the “Early Detection of Sepsis” predictive model (Verona, WI) to assist healthcare providers with early detection and interventions for sepsis patients.
A portion of this work consists of triggering a practice alert to the bedside nurse and provider when a patient meets a specific threshold score. Within the alert, healthcare providers can see the contributing factors and an assessment for clinical presentations of sepsis which are: fever, hypothermia, fast respiratory rate, fast heart rate (>90 beats per minute), altered mental status (confusion/coma) and low blood pressure or mean arterial pressure. If there are any concerns for sepsis, the nurses have a protocol to follow, and the providers have links to specific sepsis orders and proper acknowledgment actions. Since implementation, this team has been monitoring this process and has made enhancements to the threshold scores and practice alert to make it more meaningful and actional to the bedside staff.
The Sepsis Task Force continues to collaborate with the Care Design and Optimization team to work on processes to decrease variations in sepsis care and improve Parkview’s sepsis patient outcomes. Some project examples include a consensus definition of sepsis, sepsis care standards and enhancements to sepsis order sets.
More recently, Parkview implemented virtual sepsis nurses. They assist with early recognition and identification of sepsis, reduce sepsis practice alert fatigue for bedside nurses, identify subtle changes in sepsis patients and allow for extra monitoring of at-risk sepsis patients. They are constantly collaborating with bedside nurses and providers to ensure the most up-to-date care is being provided.
Implications
The ongoing sepsis work throughout Parkview demonstrates an increase in the number of sepsis diagnoses, standardized sepsis care processes and a reduction in sepsis mortality and hospital length of stay. Continuous data and outcome tracking occur to help ensure appropriate processes and proper care are in place to provide excellent care to our sepsis patients.
We will continue to enhance evidence-based practices, allowing caregivers to implement sepsis treatment to our patients more rapidly through early identification and recognition.
Did you know there are long-term effects of sepsis?
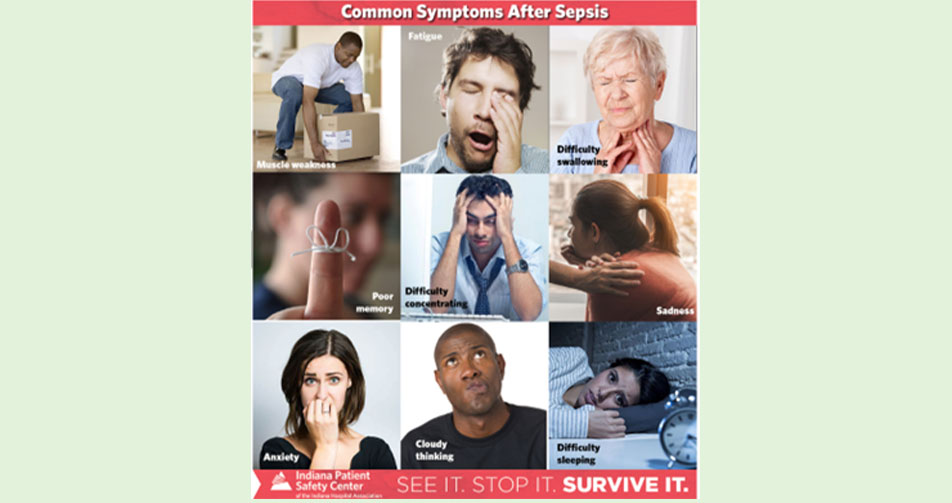
Some sepsis survivors experience post-sepsis syndrome. That means after they recover from sepsis they are left with ongoing physical and/or psychological issues, while others return to a normal life and completely recover. If you or your loved one experience any of these post-sepsis syndrome symptoms, please seek out medical care [1]:
References
[1] Indiana Patient Safety Center of the Indiana Hospital Association. Sepsis Awareness Month Toolkit SEE IT. STOP IT. SURVIVE IT. 2022.
[2] Centers for Disease Control and Prevention (CDC), Department of Health & Human Services-USA. Protect Your Patients from Sepsis. (2022).



