According to Heather Cagnet, community paramedic, Parkview Health, when it comes to sepsis, most people outside the medical community don't know what to look for. Combine that with the speed at which sepsis can progress, and you have a recipe for trouble. Heather recalls multiple cases where patients significantly deteriorate within hours. Here she explains why the condition can be confusing, what people should look for and why it’s so important to get medical care as quickly as possible.
Defining sepsis
Sepsis used to be known as "blood poisoning". While there’s a long history of sepsis, it is still difficult to diagnose. Sepsis is tricky, because there is no clear cut way to predict who will get it, and there isn’t one test to definitively diagnose it. In certain people, the body reacts to an infection, such as a UTI, pneumonia or an infected wound, with an extreme systemic inflammatory response that can lead to multiple organ failure or death.
The Centers for Disease Control and Prevention (CDC) reports that 1 in 3 people who die in the hospital do have sepsis. Those who survive can have lifelong consequences, such as organ damage, especially in the kidneys, potentially requiring dialysis, or brain damage, causing cognition issues.
Who’s at risk?
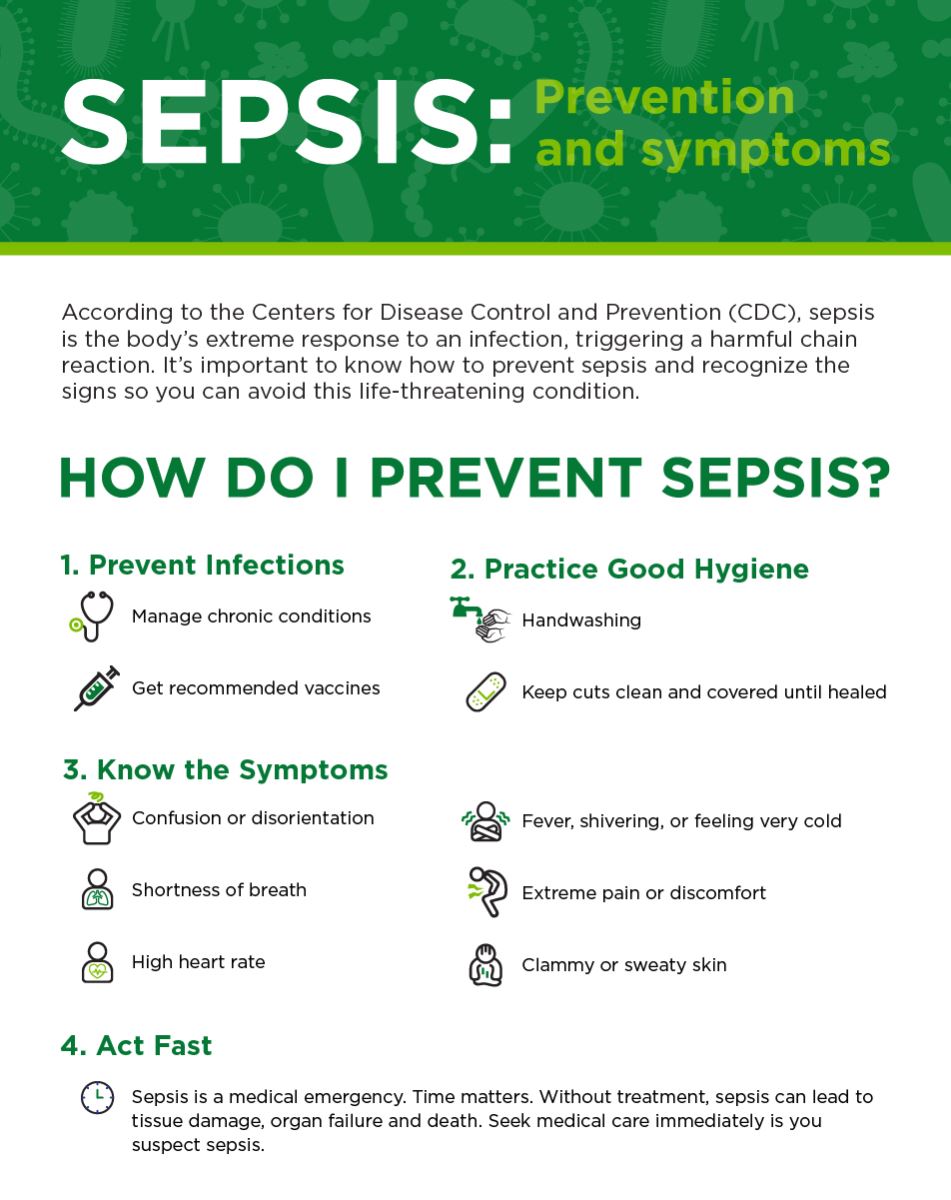
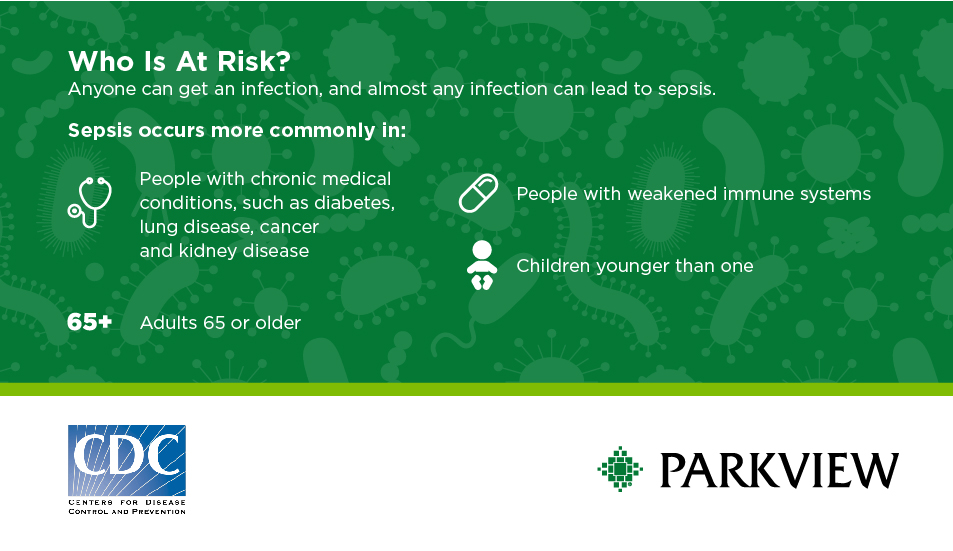
Sepsis is basically the body's extreme and overwhelming response to an infection. This means everyone has the potential to become septic, however certain subsets of the population are more likely to develop it. Babies, the elderly (65+), and those with chronic illnesses and a weakened immune system are at a greater risk.
Signs and symptoms
We have multiple tests/criteria that can clue us in to the probability of sepsis, but in most cases it is diagnosed by piecing together multiple pieces of a puzzle and ruling out other potential diagnoses.
You can refer to this helpful acronym to identify some of the signs of sepsis:
STOP AND WATCH
Seems different than usual
Talks or communicates less
Overall needs more help
Pain – new or worsening; Participating less in activities
Appetite loss
No bowel movement in 3 days or diarrhea
Drinking less
Weight change
Agitated or nervous
Tired, weak, confused or drowsy
Change in skin color or condition
Help with walking, transferring, toileting more than usual
Symptoms also include disorientation, shortness of breath, high heart rate, fever or shivering, extreme pain or discomfort, and clammy or sweaty skin.
Diagnosis
Since sepsis is a reaction to an infection, it can be difficult to pinpoint exactly when the body's normal immune response crosses the line into a life-threatening response. There are many screening tools available to help identify sepsis, and the stage the condition is in. At Parkview, we use a screening tool on patients (including every Emergency Department patient) to help identify who may be at risk. This identifies Systemic Inflammatory Response Syndrome (SIRS) in adults. If a patient is SIRS-positive, then we move to the next set of criteria.
Stages of sepsis
1) SIRS
Two or more of the following are met:
- Temperature <96.8 or >100.4
- Heart Rate >90
- Respiratory Rate >20
2) Sepsis
If a person meets SIRS criteria and has a suspected infection, then they meet sepsis criteria
3) Severe Sepsis
Sepsis criteria met and signs of organ dysfunction or a lactate level of 2 or greater
4) Septic Shock
Severe sepsis and systolic blood pressure <90, mean arterial pressure <65
Another tool we use sometimes is called the Quick Sequential Organ Function Assessment (qSOFA), which helps identify patients who have a higher mortality risk from sepsis. This looks at mental status, respiratory rate and blood pressure. A more detailed SOFA can be done in the Intensive Care Unit (ICU) setting, and utilizes other data, such as lab values. Some EMS agencies and hospitals are utilizing capnography (exhaled CO2 readings) to gather sepsis info as well, since it is noninvasive and relatively inexpensive but still gives important information.
Treatment
Treatment generally involves administering aggressive IV fluids and antibiotics, and supporting the body/organs through the entire process. Parkview has taken an innovative approach to identifying and treating sepsis early in the community by partnering with local skilled nursing facilities.
We provide education to help identify potential sepsis patients and have their nurses request the community paramedics. The paramedics start labs, IVs and treatment very quickly, right at the bedside, with the goal of turning the patient around before they become severely septic, and preventing long term organ damage and loss of life. This also hopefully saves the patient an ambulance ride and hospital stay as well.
The takeaway
While the medical community is constantly exploring new criteria and screening tools, it is so difficult to tell at exactly what point a normal immune response to an infection becomes a life-threatening event. The biggest factor in patient outcome is fast identification and treatment of the true medical emergency.
Talk to your doctor about steps you can take to prevent infections, take good care of any chronic conditions and get all recommended vaccinations. Practice good hygiene, such as handwashing, and keeping cuts clean and covered until healed. And educate yourself on the symptoms of sepsis. It’s important to act fast and get medical care immediately if you suspect sepsis or have an infection that’s not getting better or is getting worse.