
Throughout the last several weeks, there has been a little confusion and a plethora of questions as to whether people’s symptoms are that of influenza (the flu) or coronavirus (COVID-19). However, as flu season comes to a close, R. Scott Stienecker, MD, FACP, FSHEA, FIDSA, CIC, Medical Director for Epidemiology and Infection Prevention, and Joshua Kline, MD, PPG – Family Medicine, help explain the impact that social distancing is having on both the typical flu pattern and the current pandemic.
Is social distancing really working?
If the coronavirus continues to behave like the flu, social distancing efforts should be working. With that said, it doesn’t give anyone the green light to resume normal activities. By limiting exposure to others and practicing good hand-washing hygiene, we’re all helping to reduce the number of patients requiring medical care. Continuing this practice helps prevent our hospital staff from becoming overwhelmed and exhausting supplies and resources.
Numbers don’t lie
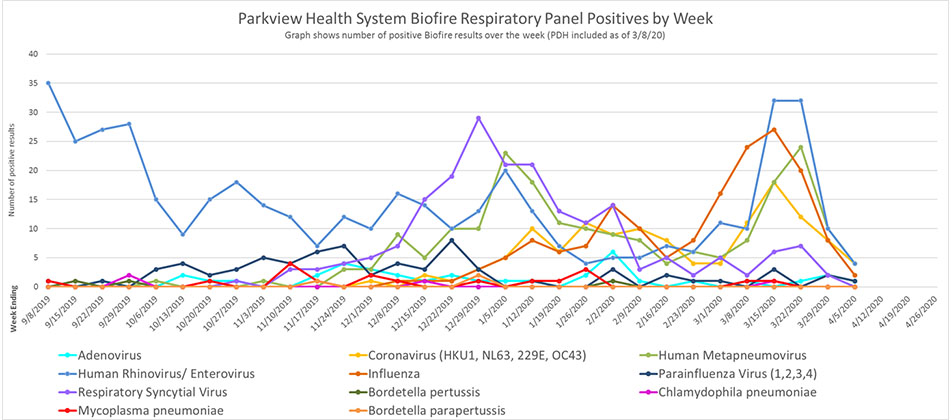
The charts below are the results of one of Parkview’s lab diagnostic systems, BioFire, and show a significant drop in respiratory illnesses in recent weeks. Historically, we’ve seen influenza season coming to an end in the springtime, but this year we’re seeing a more rapid drop in all flu-like illnesses, which can be attributed to social distancing.
However, the impact is twofold. First, we can see that social distancing is working. Clearly people are not spreading germs as much as they normally would if they were still going about their normal daily activities: work, school, sporting events, church, etc. Second, there will be less confusion as to whether a patient’s symptoms are influenza or COVID-19. With flu season ending, providers will now be able to more easily recognize potential cases of COVID-19 and act quickly to test and/or treat patients when needed.
Signs of success
It’s no secret that the flu, like COVID-19, is transmitted through large droplets expelled from a sneeze, cough or even breathing. Both viruses can survive on objects where the droplets land. People can become infected by inhaling those droplets or through contact with virus-laden surfaces or objects.
While this is not an exact comparison, flu patterns are proving to be like COVID-19 patterns. Take for example the flu numbers for the past three years:
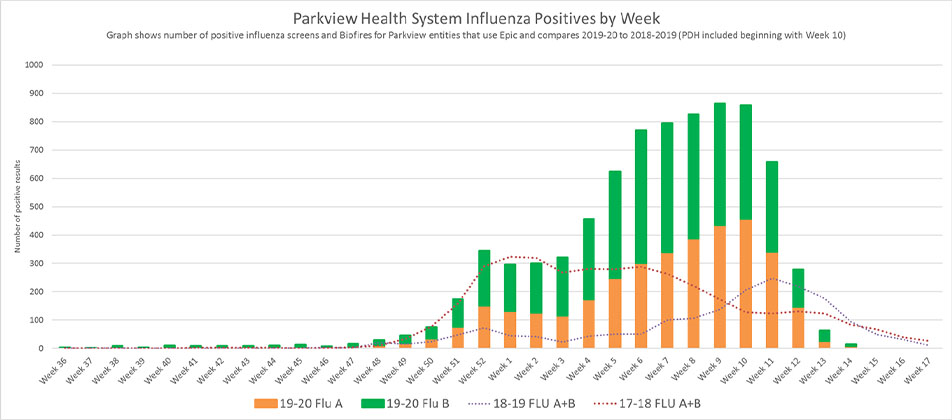
If you look at the blue dots, they show the last flu season was mild with a spike in March. The red dots are flu cases from two years ago, showing more activity and then slowly tapering off.
The orange and green bars combine both type A and B influenza, showing a busy year for flu cases but then dropping sharply, which is not explained simply by warmer weather.
This is in part due to the season, but social distancing has also played a huge role. The graphs clearing show that flu cases peaked in weeks 9 and 10 of 2020. However, as we look back we can also see that week 10 was when Indiana Governor Eric Holcomb announced gatherings larger than 250 people were banned. As restrictions grew, the flu cases shrank.
For example, the graph below shows additional respiratory cases that also seemed to drop sharply with the help of social distancing:
If social distancing is working, why should I continue the practice and follow the stay at home order?
In some cases, people won’t have symptoms until four or five days after they’ve been infected. They could unknowingly spread it to a number of people in that four-to-five-day period when they’re feeling fine. Also, about 97% of people get symptoms within 11 days of being exposed, allowing the illness to spread even when individuals aren’t exhibiting any symptoms at all.
The goal is to act as if you have the illness. Take the necessary precautions so you don't expose anyone else, especially those who could fall into the 20% of people who could get very ill and require hospitalization. Finally, please keep in mind that if we had not carried out the measures that were instituted, we would have seen a large peak that could and would have overwhelmed the healthcare system.



