This post was written by Desaray Bradley, digital copywriter, Parkview Health.
6:30 a.m.
My alarm clock went off, and the lights in my room gently faded to a scene called Mountain Breeze. It's a mix of periwinkle, pale mauve and soft yellow. Across the room, my smart speaker, in its matter-of-fact tone, announced the time, weather and my daily affirmation: "Today, I let go of my old habits and take up new, more positive ones."
Despite my inclination to plead with the tiny robot to snooze for 15 more minutes, I tossed aside my pile of covers and left the warmth of my bed to get ready for the day.
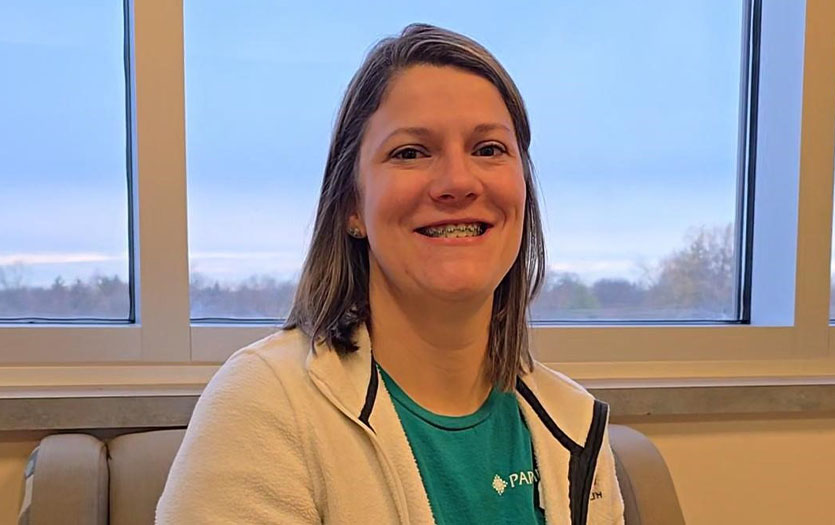
This was no ordinary copywriting day. It was my first "day in the life shadow," and I would be spending it with Caitlin Golden, a caseworker on the Mobile Crisis Intervention Team based at Parkview Hospital Randallia. This initiative, also known as the SOS program, provides immediate assistance to individuals experiencing mental health or substance use crises in 11 counties in northern Indiana.
I couldn’t help but feel both excitement and, admittedly, a small amount of nervousness as I packed my canvas bag with everything I thought I would need: a black gel pen, a moss green highlighter, my interview questions, a sticky notepad, a legal pad, my iPad and a few snacks to keep me energized throughout the day.
Before I left, I fed Flerken, my dwarf hotot rabbit and rubbed the top of his tiny head for good vibes. Feeling generous, I bit off a chunk of the apple I was holding and tossed it to him.
The morning air felt crisp. As I approached my car, I heard the faint sound of sirens in the distance and hoped they weren't an omen. Positive thoughts, Dez.
8 a.m.
When I arrived at Parkview Randallia, I gave myself a final once-over in the reflection of the backseat window. “You got this.”
I entered the hospital, waved hello to the friendly receptionist and took a seat off to the side of the lobby where we planned to meet. As I waited, I sat quietly, letting my thoughts drift. A kind smiling face brought me back–Caitlin. Right away, I could tell she was someone who made others feel safe and understood.
Caitlin escorted me past the cafeteria and through many halls–I was glad to have a guide. We arrived at her shared office full of bright sunlight, starkly contrasting the cool air outside. Three desks occupied the room, each decorated a little differently yet somehow cohesive, sharing elements that demonstrated being amongst individuals who spent their days caring for others: humorous and uplifting posters, affirmations and children's drawings.
"Make yourself comfortable," Caitlin said while booting up her computer. I slouched off my tote bag, grabbed my notation supplies and left the rest behind. Caitlin took me through the hall and introduced me to some of the other team members.
We picked up a set of keys for the shared vehicle and a shift phone to stay in touch with the team no matter where we were. At any given point in a shift, SOS team members could be at their home base, awaiting calls and assisting members of the HelpLine, or on a run, responding to a crisis on-site.
The floor buzzed with energy as some team members settled into their shifts while others wrapped up their overnight work. I could hear conversations from other small offices down the hall, playful shouts and light chatter about pending updates. Caitlin and I stopped by Heather Henry, MSN, RN, SOS program manager's office. Heather was nearing the end of a demanding overnight shift, but her energy remained steady. Her office reflected her years of experience and the depth of knowledge she possessed. It was filled with books, practical resources, personal mementos and thoughtful touches, like a table in the corner overflowing with snacks.
The night before, Caitlin attended "Dancing with the Fort Wayne Stars," a charity event at the Grand Wayne Center for The Carriage House. We listened to a speech delivered during the event by a patient discussing her journey with mental health and the challenges she overcame to become the person standing there today. The echoing testimonial drew Maggie Fleischman, Ann Williams and other SOS caseworkers into the room.
I glanced around at their faces. There were several misty eyes. I didn't know these women, but I could feel their growing emotions in the small space. They were no longer case workers; instead, generations of mothers, sisters and aunties gathered around to watch the symbolic graduation of not a patient, but someone loved by a family who wanted to see them succeed.
9 a.m.

Caitlin and Ann
I joined the team for a coffee run to the Parkview Randallia gift shop. On the way back, they received an SOS request from the Parkview Behavioral Health Institute (PBHI) HelpLine for an individual needing assistance obtaining their medication.
We settled back down in Caitlin's office. She worked on pulling up the information in the private chat and explained the typical process for receiving an SOS through the HelpLine.
In general, a person looking for help or someone acting on their behalf can call the HelpLine and speak with a Crisis Call Services Specialist. The specialist works to better understand the caller's needs and gather information for the SOS team while also de-escalating the caller if needed, similar to the role of an emergency dispatcher.
While the specialist speaks with the caller or patient via the HelpLine, the mobile crisis team collaborates with them via a group chat, either obtaining additional information on the individual in need or providing supplemental support while working towards a solution.
"When a call comes in, they'll put the patient's information in the team chat and explain what's happening. During the call, the HelpLine specialist refers to the Columbia Suicide Severity Rating Scale to assess the patient's risk. If a patient is at moderate or high risk for suicide, then a member of the SOS team will take the call from there.
Depending on the severity of the situation, sometimes we have to de-escalate before we can go out, other times we get what we need to know to keep ourselves and the patient safe and then meet them wherever they are at."
Since this wasn't a typical SOS request, Caitlin and I stayed in the office and let Maggie and Ann take the reins. In the meantime, Caitlin continued reviewing the patient's chart in case they needed additional support.
"I like to read them for my own understanding," Caitlin explained. If a patient is ever violent, aggressive or verbal in the emergency room, I like to be mindful of that, but I also like to keep in mind that we're generally engaging with them on their terms, and they want our help. They might not want to be in the ER when that behavior occurred, and they're obviously not feeling well either."
Heather stopped by Caitlin’s office for a final chat before ending her shift. The conversation turned to her early years working in the PICU with Dr. Jayesh Patel and Dr. Chandrashekhar Yalamanchali. "When they knew it would be a long night, the doctors made sure to keep the nurses fed. And I knew I had to order an onion and jalapeno pizza for Dr. Patel," she laughed.
A ping from Caitlin’s computer alerted us to a message from Ann in the group chat. It seemed their run might be turning into a crisis situation. Caitlin called Ann to get up to speed on how the interaction was progressing. She flipped from screen to screen to determine how best to provide support and updated Heather. I watched as Heather and Caitlin bounced ideas back and forth, and Ann chimed in over the speakerphone. They were sometimes listening, sometimes talking over each other, yet never missed a beat of what the other had said. While the brainstorming was energetic, it was also clear that this group functioned like a well-oiled machine.
Satisfied with their plan, Caitlin ended the call with Ann, and Heather finally made it out the door to go home. “As you can see, it's very much a team effort," Caitlin said.
Once the patient's immediate needs are met, the SOS team's subsequent goal is to guide them toward the next step in their journey. During the collaboration between Heather, Ann and Caitlin, each expressed their thoughts on the most appropriate path forward for the patient.
Later, I asked Caitlin about how she's developed that level of foresight. "Ultimately, it boils down to the patient's needs and what will help them. Going off this situation specifically, the patient probably couldn't focus on anything else until she got her medication. Now she's got them, the next priority may be ensuring she has a roof over her head. However, potential barriers to that could be a lack of transportation or not having a phone and being unable to call places that offer housing assistance. That said, I also want to ensure the assistance I offer isn't just what I think they need. Sometimes it's necessary to take a step back and gauge where they're at and what they have the capacity for."
10 a.m.
After Caitlin notated the patient's chart, we had some downtime, during which I learned more about Caitlin and the origins of the SOS team.
"When we started in 2020, it felt like we were building the ship as we went. There were only four of us, and we worked from 8 a.m. to 4:30 p.m. We weren't mobile and primarily focused on suicide and domestic violence cases. We assisted anyone who came through the emergency room, regardless of whether they were admitted. If a person was not admitted, we would follow up with a phone call or a handwritten card. If admitted, we would visit the hospital where they stayed to provide follow-up care and offer resources and support."
Although these first steps towards connecting patients to follow-up mental health care were tremendous, there was still an undeniable gap. While the medical providers in the ER could address the patients' immediate physical needs, many individuals would leave the hospital only to return to the environment that contributed to their crisis in the first place.
This also didn’t account for the many individuals who might lack access to emergency care or feel unsafe calling 911, such as those who fear law enforcement, experience stigma or are afraid of their abusers. Keeping these and other underserved populations in mind, the SOS team became mobile in 2022.
"Now we can respond in person and meet the patient where they're at," Caitlin explained. Since its inception, the SOS program has expanded to cover a broader range of mental health needs. They've also worked diligently to align with community partners like local law enforcement, schools, mental health facilities and even surrounding employers. "We go wherever we're needed."
Before Caitlin was a case manager on the SOS team, she was the lead behavioral health technician at PBHI, commonly referred to as Park Center. She explained that she had been working in the mental health field since 2013. However, she admitted that wasn't her initial plan.
"I originally went to school for veterinary medicine," she laughed. "My degree is actually in criminal justice. I thought I'd maybe go into the canine unit to work with animals and still get that criminal justice piece. But when I graduated, I ended up in mental health."
Caitlin shared that she's passionate about the career path for several reasons, including the fact that she's been personally affected by suicide. The small semi-colon tattoo on her wrist stands out a little more with this admission.
"Mental health is very real and just as important as physical health. I think that has impacted where I am and my passion for helping others better themselves. People are not defined by their diagnosis."
When not on a call or in the community, Caitlin's downtime is often spent catching up on training, coordinating the team's schedule and managing patient cases. Case management looks like bridging the gap from crisis to getting the individual established on an outpatient level and keeping them out of the hospital. However, that can be met with challenges beyond what the patient can handle independently.
"Following up with someone from that initial crisis, we try to help them address any barriers we can. We want to ensure their basic needs are met, then work on getting them connected to mental health care."
Caitlin emphasizes the importance of keeping the patient's interests top of mind. "We ask them what they want and where they want to go. It doesn't do them any good to set them up with resources if they aren't interested in or can't access them."
Because the SOS team responds to 11 surrounding counties–including Allen, Adams, Dekalb, Huntington, Kosciusko, LaGrange, Noble, Steuben, Wabash, Wells and Whitley counties–that involves coordinating care that's closest to the patient, helping them secure transportation or informing them of virtual options.
11 a.m.
"Caitlin, we're getting a call," Maggie's voice came from the hallway, "and it's complicated." She appeared in the doorway, looking slightly flustered, and quickly outlined the situation.
A family member was calling the HelpLine regarding their loved one. The patient's employer reached out to the patient’s family because they had been exhibiting concerning behaviors at work after recently struggling with their mental health. However, the individual was not in a state of mind to call on their own.
Caitlin immediately pulled up the patient's medical record. I watched as she navigated the system, her pace purposeful but methodical. Maggie stood beside her, offering additional context gleaned from her brief conversation with the family member.
Where I saw fragmented details and clinical jargon, Caitlin and Maggie identified patterns and concerns. Caitlin pointed out recent inpatient stays, the symptoms the patient experienced and medications they had been prescribed, gathering a comprehensive understanding of their health status.
Because the individual in potential need of support was not the caller, Maggie and Caitlin discussed options for approaching the situation as delicately as possible to ensure the safety and comfort of everyone involved. "I would let the family member know that we would recommend coming to see the patient and not waiting for something to happen," Caitlin said to Maggie. She continued reviewing the patient's history to prepare for the possibility of intervening.
A short while later, Maggie returned after connecting with the patient's manager. Caitlin took notes as Maggie relayed their concerns. The manager wanted to support the employee but was uncertain how to approach such a complex topic without escalating matters unnecessarily.
Maggie coached them through a measured response, emphasizing compassion and understanding. Caitlin added further guidance, suggesting they "Start with reassurance. Say something like, 'We care about you and want to help.'"
While the team ultimately determined that an immediate on-site visit wasn't necessary, Caitlin reminded me that support over the phone can be just as impactful as an in-person intervention. "This kind of guidance gives those closest to the individual the tools to manage these interactions effectively," she explained. "In these cases, we just have to leave a paper trail."
While much of the SOS team's work happens in the community, these records create a roadmap for the next time this person, or anyone in similar situations, seeks help, ensuring no one is left behind.

12 p.m.
After two calls but zero interventions, Caitlin and I examined previous cases she'd worked on over the years. Using a template modeled after other crisis intervention teams, SOS caseworkers keep a detailed narrative of each patient interaction within their medical records.
"We capture everything. It can get lengthy, but it's a crisis note. It touches on their thought processes, any thought disorder, paranoia, hallucinations, delusions, suicidal ideation, homicidal ideation, substance use," she said, pointing to each check box. "So we can tie it all together in our notes and explain what happened and what led them to their crisis. We also include if the patient has had a history of mental health services or any barriers to treatment. I really like this section because it's easy to come back to and can help us determine what's preventing them from moving forward."
I asked about how tools like the Columbia Suicide Severity Rating Scale contribute to their assessments. Caitlin paused, "Let me pull up another one."
Her tone shifted, becoming quieter, more reflective. "There's nothing I could have done, but I'm still kind of kicking myself," she said. "This patient was screened low risk. However, it was kind of like a perfect storm. There were a lot of red flags and stressors that could have caused the patient to go from low to high risk very easily ... and they did. They attempted [suicide] the next day."
Caitlin described more components of the patient's circumstances that led to their mental health crisis. A difficult family situation, loss of employment, unenrolling in school and a family history of mental illness. Each of these factors contributed to the patient's overall risk, even though the formal assessment didn't reflect immediate danger.
While tools like the Columbia Suicide Severity Rating Scale have proven to be among the most accurate, the work of mental health professionals will always be complicated by factors that are largely out of their control. This is why the SOS team’s in-person interventions are so critical.
1 p.m.
"Are you hungry?" Caitlin asked as she wrapped up the morning's work. We decided to head to a local Thai restaurant on State Street.
While we waited for our food, Caitlin received a message in the group chat. "Sometimes this job means working while you eat," she said quickly, tapping out a response. "I try to leave work at work when I can, but if a call comes in, I have to respond."
Our conversation shifted back to what risks can look like and how to help someone in crisis. I asked Caitlin about recognizing the signs and what to do if someone's behavior points to a mental health crisis.
"If someone's at all concerned or has questions, I'd recommend calling," she said. "Even if it's just for guidance. The HelpLine can connect the caller or person to our team or provide support directly. That could look like screening them or just giving advice. Whether or not someone thinks the situation is serious, it's always best to take it seriously."
2 p.m.
After lunch, we returned to the office to check-in. The early afternoon was quiet, allowing us to step away from case management for a bit. Caitlin suggested we visit the Park Center campus. The sun had finally come out, casting a golden hue over the grounds and providing suitable conditions for a brief walk around.
The SOS team has a strong relationship with Park Center. In addition to receiving mobile intervention requests from PBHI, in some instances, the SOS team will bring a patient directly to the Park Center campus after a crisis intervention and aid in the intake process, allowing for a smooth transfer of care.
As we got back to the car, Caitlin turned to me and asked, "Do you want to go on a call?" A request for intervention had just come through the group chat.
3 p.m.

Sara and Caitlin
By the time we made it back to Caitlin's office, Sara Dill, lead caseworker, was waiting for us. She gave us an overview of the patient's circumstances. We quickly grabbed our things and were out the door. Speed-walking through the halls, Caitlin shared that a therapist reached out to the HelpLine on behalf of a patient they were concerned might harm themselves.
The sun was no longer shining. Overcast clouds and chilly air ushered us out the side door, onto the street and towards a grey Dodge minivan in the parking lot.
Caitlin climbed into the driver's seat. Sara offered me the front passenger seat, and she took the middle row. Sara worked from her laptop, preparing her notes as we drove across town. The time traveling to the patient is often spent strategizing.
"This patient already participates in an intensive outpatient program (IOP), but, per their therapist, they might need to come in. So we'll go see where they're at. The whole idea is that by the end of the interaction, we can have a plan in place that they're on board with and that keeps them safe. But if they don't feel like they can keep themselves safe and need to come in, we support that too," Caitlin said.
Caitlin and Sara spent the remainder of our drive reviewing the patient's chart aloud, working ten steps ahead to anticipate their needs and how best to provide support.
4 p.m.
We arrived at the patient's home. They didn’t come to the door immediately. On the other side, we could hear a small dog barking in the background. We waited. I was anxious, unsure if my nerves were tied to the impending interaction or the fear we were too late. I pushed aside my negative thoughts. Caitlin knocked again, and there were more small barks and rustling behind the door.
A middle-aged woman and a chihuahua appeared in the frame. Caitlin introduced us, and the woman, although seeming hesitant, stepped aside to let us in. She apologized for the condition of her home. I sympathized with her look of embarrassment over unexpected guests catching one off guard.
We sat in the patient’s living room, Caitlin to my left and Sara to my right. They unpacked their laptops and got into their flow. Caitlin worked through the Columbia screening. "Have you wished you were dead or wished you could go to sleep and not wake up?"
The questions hung heavily in the air between drawn-out pauses while the woman struggled to get her words out. Caitlin and Sara were patient and encouraging. When Caitlin noticed the woman became overwhelmed, she redirected the conversation to the patient's playful dog or the shy, long-haired cat that later introduced herself by perching on my lap.
I found it funny how pets always think that visitors are, of course, there for them. I suppose, in a sense, we were–ensuring their owner's safety. I think they were happy we were there.
Through these light interactions, the patient's demeanor changed. She laughed and smiled in a scenario that could easily register as somber. Slowly, she shared more about what had been going on in her life.
Due to changes in care with her in-home assistance, she didn't have access to transportation and had become disconnected from recreational activities and social interaction. This isolation was further exacerbated by the recent death of a close friend and not being able to travel to and attend their funeral services.
Caitlin and Sara worked together to offer solutions that would help the patient move forward. They provided resources for transportation and grief support and made plans to follow up with the patient's mental health provider.
Because the woman was currently involved in mental health services, she already had safety plans in place, which Caitlin and Sara reviewed verbally. In other scenarios, the caseworkers would fill out the behavioral health safety plan with the patient and give them a copy to keep as a reminder and one to have on their medical file for future reference. The form references:
-
Common warning signs that a crisis may be developing.
-
Coping techniques I can use to take my mind off the problem.
-
Places or social settings that provide distraction, help me feel better, or offer support.
-
Names and numbers of family or friends I can contact.
-
Things that make my environment safe.
-
One thing that is most important to me and worth living for.
Although the patient was able to overcome the initial crisis with guidance from Caitlin and Sara, she decided, for her safety, to relinquish her medication supply and maintain enough to get through the weekend. Caitlin and Sara assured her they would follow up with her on Monday.
Before we left, Caitlin and Sara encouraged the woman and reminded her that the crisis team was only a call away should she need additional assistance.
6 p.m.
Once settled back into the car, I felt a mix of relief and what I'd describe as second-hand accomplishment. The visit with the patient had been tense at moments, but Caitlin and Sara handled it with professionalism and care.
Caitlin, driving us back, asked me, "Well, what did you think?". It was a lot to process. While I anticipated an on-site response, I wasn't sure what it might entail. "It's interesting," I replied. You truly never know what you're going to walk into."
After more time reflecting on my observation, I can say I have immense respect for the SOS caseworkers' ability to think on their feet and pivot when needed. While a patient's chart can detail how their mental illness has or may manifest, it cannot fully capture the variability of the human experience.
In turn, I asked Caitlin how they develop their recommendations during an intervention. "Well, safety is always the number one priority," she said, echoing a sentiment she had shared numerous times throughout the day. This typically begins by identifying the most immediate risk to the individual. In other words, what they have access to that they might use to harm themselves.
"For this patient, she admitted pills were her method. While I'd usually want to cover all pills, her specific method was her prescription medication. As far as any additional support goes, it's case by case. We suggested grief support, but we also have to consider if it's helpful to add on another therapist or if it's something she could process with her current therapist. I also don't want to set something up for her while she doesn't have reliable transportation. So, in this situation, securing the medication and helping her get home health back is most beneficial."
Caitlin and Sara discussed options for another case manager to check in on the patient over the weekend, ensuring she had support until she could connect with her regular mental health provider.
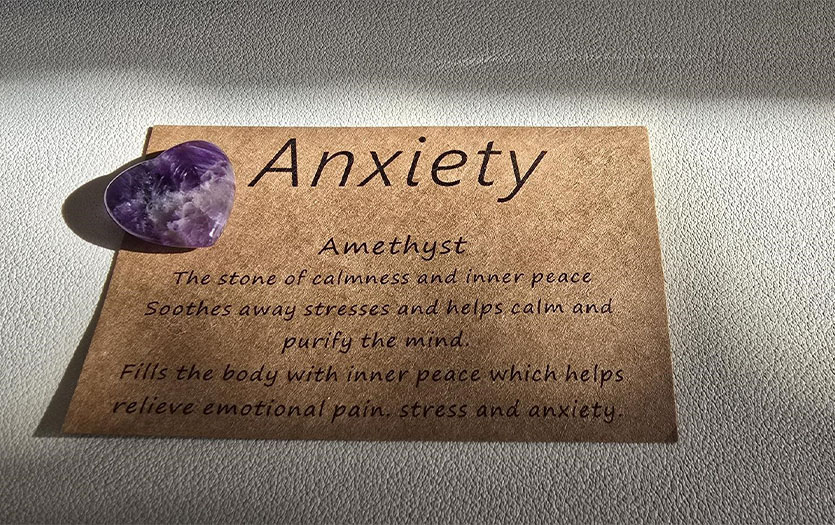
Once we were back at the office, Caitlin advised that the final steps for the evening would be entering the patient's notes with Sara and safely locking away the secured medication. I offered to stay, but she assured me I wouldn't miss anything crucial and encouraged me to get home. Before we parted, she offered me a small gift: a purple heart-shaped amethyst stone with a note on anxiety.
“Amethyst: The stone of calmness and inner peace soothes away stresses and helps calm and purify the mind. Fills the body with inner peace, which helps relieve emotional pain, stress and anxiety.”
I thanked her for the memento, and she walked me back down to the parking lot so I could head home.
Closing thoughts
On my drive back to my apartment, I decompressed. The radio was humming in the background, but I wasn’t listening. I found myself thinking about the woman we had just left.
It took courage to allow strangers into her world during such a vulnerable time. I glanced over at my amethyst heart and promised myself that if I ever found myself in such a moment of need, I would do my best to summon even a fraction of that bravery, trusting that people like Caitlin and the SOS team would be willing to walk beside me.
If you or anyone you know is in need of help, call the PBHI HelpLine at 260-471-9440 or 1-800-284-8439 to be connected to the SOS team or other services 24 hours a day, seven days a week.



