
Sepsis is a global healthcare problem, affecting more than 47 million people and taking more than 11 million lives every year. Of those cases, 40% affect children under the age of five. This means there is a sepsis-related death every 2 minutes. [1] Jennifer Rechter MSN, RN-BC, AG-CNS, sepsis coordinator, Parkview Health, tells us more about this condition and what Parkview is doing to minimize instances of sepsis.
September has been recognized as National Sepsis Awareness Month by the Sepsis Alliance. The goal is to increase knowledge and awareness on sepsis, not just to those in the medical field but also to families, patients and communities. This is particularly important, as around 80% of sepsis cases are acquired outside the hospital, making it a public health issue, not just a condition the hospital needs to address. [1]
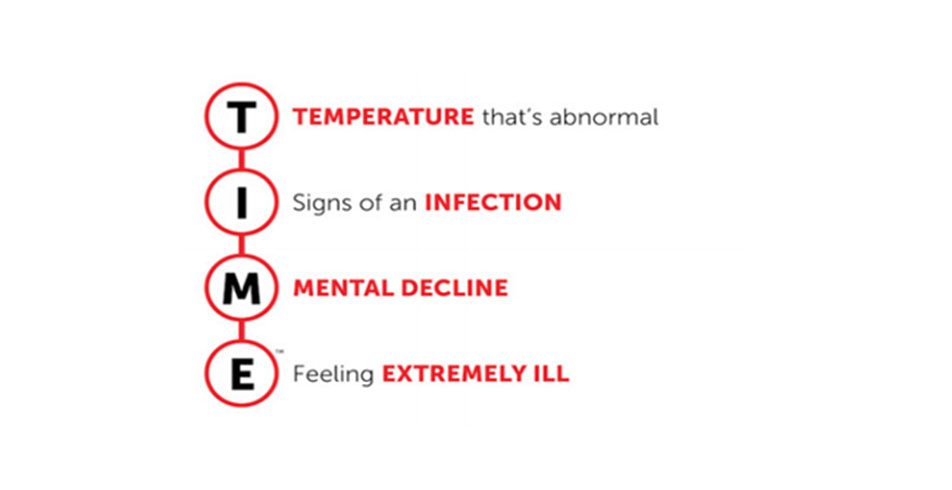
To aid in this goal, the Sepsis Alliance asks that we all come together to support the effort and save lives by promoting sepsis awareness. We can all do our part by taking TIME to learn more about sepsis and knowing the signs and symptoms of the condition. [1]
What is sepsis?
Sepsis is the body’s overwhelming and potentially life-threatening response to an infection, which can lead to tissue damage, organ failure and even death. [1]
Who is at risk for sepsis?
Sepsis can affect anyone, but according to the Centers for Disease Control and Prevention (CDC), some populations are at a higher risk. [2] Specifically, those who:
- Are under the age of 1 or over age 65.
- Have a weakened immune system or chronic illness (diabetes, cancer, kidney, liver disease, splenectomy, dialysis, etc.).
- Have a severe burn or wound.
- Have an indwelling catheter or IV.
- Recently had surgery or have been hospitalized.
What causes sepsis?
Any infection can lead to sepsis. Here are the four most common infections associated with sepsis [1]:
- Lungs (pneumonia)
- Kidney (urinary tract infection)
- Skin (new or worsening injury or wound)
- Abdomen or gut
What are the signs or symptoms of sepsis?
Unfortunately, there is no single sign or symptom because sepsis can occur from any infection. With that said, diarrhea, vomiting and a sore throat are the most common indications of an infection. Additionally, those suffering from sepsis might also experience the following [1]:
- Shivering, fever, feeling very cold
- Extreme pain or feeling worse than ever
- Pale or discolored skin
- Sleepiness, difficulty waking up, confusion
- I feel like I might die
- Shortness of breath
What is Parkview doing to identify sepsis early?
In January of 2019, the Sepsis Task Force team, in collaboration with the Business Intelligence-Analytic team, implemented the “Early Detection of Sepsis” predictive model (Verona, WI) to assist healthcare providers with early detection and interventions for sepsis patients. A portion of this work consists of triggering a practice alert to the bedside nurse and provider when a patient meets a specific threshold score. Within the alert, healthcare providers can see the contributing factors and an assessment for clinical presentations of sepsis which are: fever, hypothermia, fast respiratory rate, fast heart rate (>90 beats per minute), altered mental status (confusion/coma) and low blood pressure or mean arterial pressure. If there are any concerns for sepsis, the nurses have a protocol to follow, and the providers have links to specific sepsis orders and proper acknowledgment actions. Since implementation, this team has been monitoring this process and has made enhancements to the threshold scores and practice alert to make it more meaningful and actional to the bedside staff.
The Sepsis Task Force continues to collaborate with the Care Design and Optimization team to work on processes to decrease variations in sepsis care and improve Parkview’s sepsis patient outcomes. Some project examples include a consensus definition of sepsis, sepsis care standards and enhancements to sepsis order sets.
More recently, Parkview implemented virtual sepsis nurses. They will assist with early recognition and identification of sepsis, reduce sepsis practice alert fatigue for bedside nurses, identify subtle changes in sepsis patients and allow for extra monitoring of at-risk sepsis patients.
Implications
The ongoing sepsis work throughout Parkview demonstrates an increase in the number of sepsis diagnoses, standardized sepsis care and a reduction in sepsis mortality. Continuous data and outcome tracking occur to help ensure appropriate processes and proper care are in place to provide excellent care to our sepsis patients.
We will continue to enhance evidence-based practices, allowing caregivers to implement sepsis treatment to our patients more rapidly through early identification and recognition.
References
[1] Indiana Patient Safety Center of the Indiana Hospital Association. Sepsis Awareness Month Toolkit SEE IT. STOP IT. SURVIVE IT. 2020.
[2] Centers for Disease Control and Prevention (CDC), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Health Quality Promotion (DHQP). What is Sepsis? 2021.



