This post was written by Jonathan Shirazi, MD, PPG – Cardiology.
As we continue to see cases of COVID-19 in our area, we also continue to learn more about the effects of the virus, both during active infection and in the weeks and months that follow.
Elevated risk
We know that there is an increased risk of severe illness for those who have:
- congestive heart failure
- coronary artery disease
- pulmonary hypertension
- hypertension
- diabetes mellitus
- obesity
- chronic kidney disease
- COPD
- Smoking
- sickle cell disease
- Down syndrome
- cancer
We are also seeing people delay their cardiac care, which increases their risk of a more negative outcome related to a cardiac event. If you are having chest pain, significant shortness of breath, passing out, or experiencing new significant symptoms, seek medical attention. It’s also imperative that you keep up with routine preventative screenings to catch any cardiovascular issues early.
We have seen patients avoiding the Emergency Department or clinic visits in order to prevent COVID-19 exposure. Unfortunately, many of these patients end up having a heart attack or even passing away at home. There are many safety protocols in place to protect staff and patients at our facilities. Please, do not wait to seek care.
How COVID-19 affects the heart
The ACE2 receptor is the primary mode for the novel coronavirus entering our cells. While this process is present in the respiratory tract, it is also present in myocardial cells, therefore, one working hypothesis is that there is direct viral invasion and injury to the myocardium (muscular tissue of the heart) with COVID infection. This is referred to as myocarditis. Myocardial injury can also be caused by stress from the active infection as well as injury from an overly aggressive inflammatory response (cytokine storm).
There are several cardiovascular presentations with acute COVID-19 infection, including:
- Myopericarditis – Abnormal electrocardiogram (ECG) changes; symptoms including chest pain and shortness of breath
- Worsening of pre-existing heart failure, atrial fibrillation and other cardiac conditions
- Cardiogenic shock
Complications during and following infection
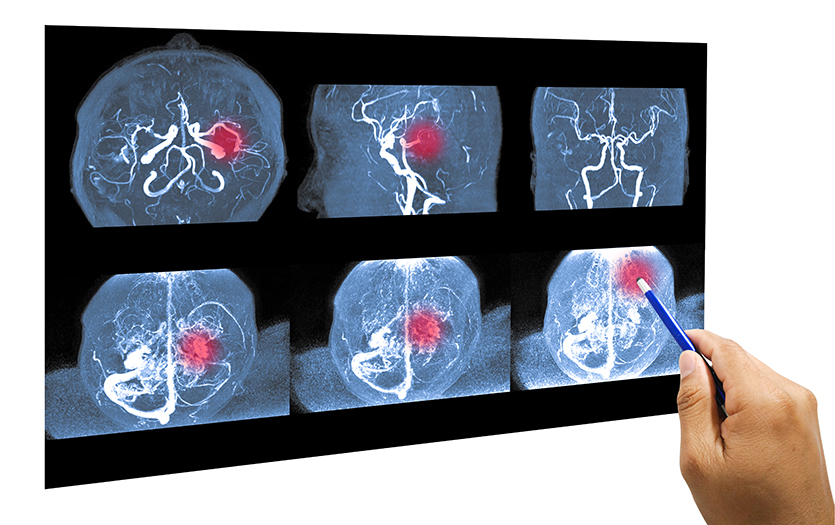
During the acute COVID-19 infection and in the few weeks following the respiratory illness recovery, we’re seeing thrombogenic/thrombotic problems (clotting). This means that people are having heart attacks, strokes, and other blood clots in the lung or even in other organs.
In addition, we’re seeing:
- Patients who had myocarditis are sometimes developing heart failure
- Patients who had myocarditis are struggling with arrhythmias after recovery
- Atrial fibrillation
- Premature ventricular complexes
- Non-sustained ventricular tachycardias (NSVT)
- Changes in autonomic tone, manifesting as higher resting heart rates
Some patients are noticing faster baseline heart rates and faster heart rates with mild activities. Some are experiencing dramatic symptoms like shortness of breath and dizziness walking from one room to the next. We’ll hear from some patients who were really active, got COVID, and now, instead of a resting heart rate of 60, their resting heart rate is 90 and getting up to 120 when they walk short distances. This is something electrophysiologists have seen with other viruses, too. Some viruses reset your heart rate. Typically, the issue will resolve in up to 12 months. If they feel dramatically worse, there is medication that can help.
While we know that the risks are higher for patients who have had heart disease, the risk for cardiovascular event, stroke and heart attack go up dramatically for all populations. Additionally, those who are obese, have diabetes, heart failure and/or arrhythmias are at risk for intensifying the existing disease. These risks are higher during acute infection, but the overall threat can extend up to six weeks after the initial illness.
So where is this risk coming from? Well, a few things happen when we get a viral infection. First, we have two inflammatory markers, cytokines and interleukins. One of their jobs is to “rev up” the immune system. But as you reach certain thresholds of some specific cytokines and interleukins, it can change how ion channels function within the heart. They can alter how our heart actually beats, recharges and prepares for the next beat. This can, but doesn’t always, translate into an arrhythmia.
Additionally, when the inflammatory response is extreme, there is an increased chance that the body will activate a clotting cascade, meaning the body will form clots when it’s not supposed to. Increased clotting means an increased risk of pulmonary embolism, stroke and even heart attacks.
Independent from that, because the virus infects cells through ACE2 receptors primarily in the lungs but also in the heart, during acute infection, the virus has access to the actual muscle cells in the heart. Thankfully, for the majority of people, this is uncommon or only to a small degree. However, there is one autopsy study that demonstrated that 60% of individuals with severe disease show that the virus invaded the heart muscle.
When to seek medical assistance
If an individual notices that their heart rate is substantially faster than usual and they are having symptoms, it’s important that they see a medical provider to rule out potential complications. We often have patients who notice an issue because their smartwatch indicates a higher or erratic heart rate. This higher heart rate will often resolve on its own, but not always. And it can be a sign of something more alarming.
If a patient is experiencing symptoms such as dizziness, light headedness or they are short of breath with an elevated heart rate, we want to rule out heart failure. Patients should also seek immediate evaluation if they notice chest discomfort, palpitations or pounding.
Generally speaking, if a patient’s symptoms are not improving week-to-week they should be evaluated. Similarly, if symptoms are lasting longer than four weeks, the patient should seek medical attention.
People recover from the COVID-19 virus at different paces. In most cases, symptoms are associated with a deconditioned heart, which is why they have the elevated heart rate. They need time to heal and get back into their normal activities. But it’s best to get a medical opinion.
Recovery
If an individual had COVID-19 and is working on recovery, the goal should be to keep the heart rate the same for a duration of time. If your heart rate is elevated and you are short of breath, you want to stay at that point for several minutes to help recondition the heart. This is also called interval training. You want to get to the point of experiencing symptoms and stay there for 5-10 minutes. Don’t try to push past. Then take a little break. It’s important to note that if you are light headed, you need to stop.
The heart rate is a nice piece of data to have but it’s very individualized from person to person. Someone might get their heart rate to 170 with no symptoms and be able to maintain. Someone else might get to 140, experience symptoms and need to stop. The symptoms are the indicator.
Also, the trajectory, or rate of acceleration, of the heart rate matters more than the actual number. A slow, steady rise is normal, but if your heart rate is lower, then jumps, that could indicate an abnormal rhythm. Wearables, or heart rate tracking devices are a great way to follow these trends.
Precautions
Pandemic precautions include:
- Getting vaccinated as soon as it is available to you
- Wearing a mask
- Minimizing exposure (outdoor visits with better airflow are less of a risk than indoor)
- Washing your hands
Anyone, with or without cardiovascular disease, should get the COVID-19 vaccine. While there are extremely rare complications from the vaccine, we are seeing a substantial amount of complications from the virus.
Individuals who get the vaccine have two layers of benefit. First, they have some protection against getting the virus. Second, even if they acquire the virus, the symptoms and recovery time are dramatically reduced. They are far less likely to have symptoms that require going to the hospital, being in the ICU or, in worst case scenarios, dying.
If a patient already has cardiac disease, it is safe to get the vaccine. Any of the vaccines that are currently available are better than none, so I recommend getting the first one available to you.
I know that most of us want things to go back to “normal.” In order to get there, we have to have widespread vaccine use. If we don’t, a small amount of the virus will linger in society. Viruses mutate, so we may very well end up having these restrictions for a longer period of time. If we already know the vaccine is less risky than the virus, and it benefits society, it’s hard to argue against getting the vaccine.