
This post was written by Mark O'Shaughnessy, MD, PPG – Cardiology.
The heart is an intricate muscle. When everything is pumping and flowing as it should, the organ can be a powerful engine for the body. When the anatomy is altered, however, patients can experience concerning symptoms and even the risk of a catastrophic health event. In this post, we will explore a category of conditions with a genetic componenet than can cause concerning complications.
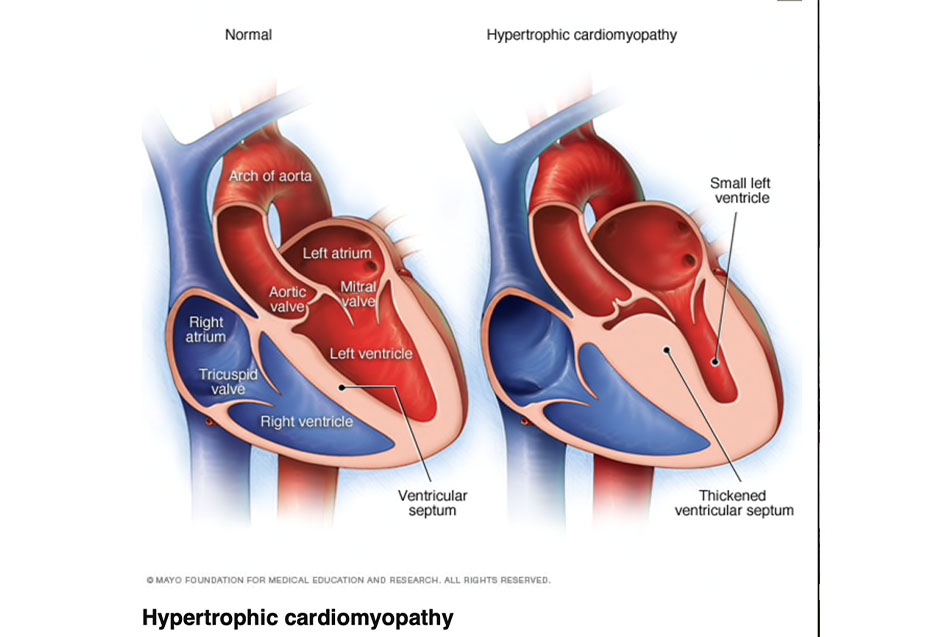
Hypertrophic Obstructive Cardiomyopathy (HOCM), Asymmetric Septal Hypertrophy (ASH), Hypertrophic Cardiomyopathy (HCM) and Idiopathic Hypertrophic Sub-Aortic Stenosis (IHSS) are all terms for an abnormally thick heart muscle that can have significant clinical implications.
What is hypertrophy?
The heart is a very sophisticated muscle that consists of four chambers (two upper: atria and two lower: ventricles). Like any muscle, if you exercise the muscle the muscle responds by growing (hypertrophy). There are normally two types of hypertrophy.
The first is eccentric hypertrophy. This is when the muscle cells get longer (elongate) allowing for a larger chamber. We typically see this in response to aerobic/endurance exercise. Eccentric hypertrophy improves the output from the heart (cardiac output) and is considered a beneficial type of hypertrophy.
The other is concentric hypertrophy. This type is the result of high blood pressure or increased resistance to outflow, like we would see with aortic valve disease, which increases the workload on the left ventricle (lower chamber on the left) causing it to become thicker. Concentric hypertrophy is considered a detrimental form of hypertrophy.
A third type of hypertrophy
With hypertrophic cardiomyopathy, on the other hand, patients have an inherited form of thick heart muscle not in connected to exercise or hypertension. The abnormality occurs because of a mutation in a specific gene in the DNA of the affected individual. This encodes abnormal development and structure of the heart muscle.
The abnormal thickness occurs typically in the intra-ventricular septum (the wall between the two lower chambers), and results in a narrowing of the outflow tract (the area where blood from the left ventricle converges on its way out of the heart). This causes obstruction to flow from the heart.
In addition to the obstructed blood flow, the muscle cells are not oriented in the normal fashion (nice parallel bands), but rather have a somewhat chaotic orientation to each other, which can alter the electrical signal that allows the heart to work efficiently and can create life-threatening rhythm disturbances. We see this when athletes die suddenly while participating in their sport. This is often due to undiagnosed HCM.
Diagnosing Hypertrophic Cardiomyopathy
Symptoms
Hypertrophic Cardiomyopathy is typically identified because of a heart murmur (turbulent blood flow heard with the stethoscope), or the presentation of symptoms that include shortness of breath, chest pain, fatigue, dizziness and/or passing out (syncope). These symptoms will trigger the primary care provider or cardiologist to order an echocardiogram (cardiac ultrasound) which can identify the abnormal thickness in the septum along with the identification of the associated outflow tract obstruction.
Evaluation
Once the anatomic abnormality has been identified, it’s important to evaluate the patient for possible abnormal heart rhythms (premature ventricular contractions, ventricular tachycardia or ventricular fibrillation) as these can be life-threatening and need to be aggressively treated. Typically, a heart rhythm monitor (holter or event monitor) will be ordered to identify those individuals at risk for serious rhythm complications associated with the disorder.
Preventive Screening
Since HCM is a genetic abnormality inherited from parents, it’s important to screen the offspring of any affected individual to assess their risk of developing the disease. Fortunately, with the availability of genetic testing, we can identify individuals who are at risk for the development of the abnormality and can follow them closely, prepared to treat the condition before there is a poor outcome. The team at Parkview Heart Institute’s Cardiovascular Genetics Clinic can screen affected families and follow those individuals who exhibit the gene mutation, as well as many others that can create cardiac abnormalities.
Treating Hypertrophic Cardiomyopathy
Treatment of HCM includes medications that can help with the outflow obstruction and suppress abnormal heart rhythms. In certain circumstances, patients need a fancy pacermaker called an Internal Cardioverter Defibrillator (ICD), which monitors the heart rhythm and will either pace or shock the person out of the abnormal rhythm. Think of the ICD as a “guardian angel” who watches over the patient and steps in if it identifies a serious life-threatening heart rhythm.
Once the abnormality has been identified, it’s important that the affected individual is followed closely by a cardiologist with knowledge and expertise in the management of HCM and its complications.
If you are experiencing any of the symptoms mentioned above or have a family member who has been diagnosed with HCM, speak with your primary care provider or cardiologist to explore a treatment plan.



