This post was written by Rakesh Subramanian, MD, FCCP, Pulmonologist/Critical Care Physician – Parkview Physicians Group.
ECMO is a type of artificial life support that can help a person whose lungs and/or heart aren’t functioning properly. Decisions around when to use ECMO and when to take patients off are complex. Let’s shed more light on this tool and the details around its use.
What is ECMO?
ECMO, short for Extracorporeal Membrane Oxygenation, is a sophisticated medical procedure evolved from the cardiopulmonary bypass machine. It's designed to aid patients whose heart and/or lungs are failing beyond the capabilities of conventional treatments. By using large cannulas (tubes) inserted into major blood vessels, ECMO draws blood from the patient, enriches it with oxygen, removes carbon dioxide, and then returns it. This process can support lung function (veno-venous ECMO) or both heart and lung function (veno-arterial ECMO).
Watch this video for a better understanding of ECMO.
What types of conditions is ECMO used for?
ECMO is a critical intervention for patients with severe respiratory or cardiac failure who haven't responded to standard treatments. Serving as a bridge to recovery, transplantation, or other support devices, ECMO can manage a wide range of life-threatening conditions. These include pneumonia, acute respiratory distress syndrome (ARDS), pulmonary hemorrhage, severe asthma/COPD exacerbations, various forms of shock, and cardiac arrest.
How long can a person stay on ECMO?
Typically, ECMO is a short-term solution, providing crucial time for recovery. Patients can be supported for several months on veno-venous ECMO if they show potential for recovery or are awaiting a transplant. Veno-arterial ECMO support generally lasts a few days.
What are the risks when using ECMO?
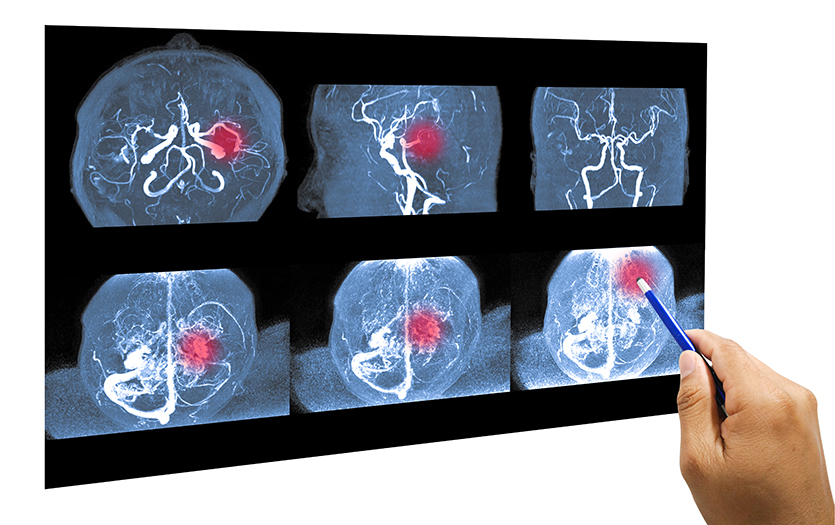
While ECMO can be lifesaving, it's not without significant risks. These include major bleeding, infections, limb complications, blood clots, stroke, air embolism, damage to blood vessels and heart, hemolysis, transfusion-related issues, and in some cases, death. ECMO is therefore reserved for patients who are not responding to, or are unlikely to respond to, standard treatments.
What is the process for coming off ECMO?
The process of weaning a patient off ECMO begins when their heart or lung function improves. The ECMO support is gradually reduced, and if the patient can maintain their lung and heart function with minimal assistance, ECMO is discontinued.
Coming off ECMO is the start of a longer recovery journey. Patients typically require continued conventional support, like mechanical ventilation, antibiotics, and blood pressure medications. A prolonged period of rehabilitation is often necessary to regain physical strength.
Are there any long-term effects from being on ECMO?
Long-term health issues can arise for ECMO patients, many of which are related to their underlying severe illness. These may include fatigue, muscle weakness, neuropathy, limb circulation problems, cognitive impairment, anxiety, depression and ongoing organ failure requiring long-term support.
While ECMO can be crucial, it's important to understand its role in supporting, not curing, the underlying condition. Its initiation and discontinuation involve complex decision-making by a multi-disciplinary team. The journey through and beyond ECMO can be challenging, with uncertain outcomes. Active involvement of patients and families in these discussions is vital, and our team at Parkview is committed to guiding and supporting them every step of the way.
If you notice any changes in your respiratory health, be sure to make your primary care provider aware so they can investigate your symptoms and refer you to a pulmonologist if necessary.