
This post was written by Jithmie Jayawickrema, PT, Parkview Therapy Services, and Sean Collins, PT, Parkview Therapy Services.
If you’re experiencing discomfort and limited mobility in your shoulder, it could be this common joint diagnosis.
Defining frozen shoulder
Frozen shoulder, also called adhesive capsulitis, is a painful shoulder condition with progressive limitations in shoulder range of motion and mobility. Changes to the fibrous tissue (fibrotic changes) and a permanent shortening (contracture) of the glenohumeral joint (the ball and socket joint in the shoulder) can be seen in patients who have been diagnosed with frozen shoulder.
Causes
While the exact cause of frozen shoulder is not clearly understood, evidence shows that it can be related to diabetes, hypothyroidism and some autoimmune diseases. Females, individuals ages 40-65 and people with a history of adhesive capsulitis in their other shoulder are also predisposed to the condition.
While primary adhesive capsulitis is insidious by nature, secondary adhesive capsulitis is related to prolonged immobilization, seen post-op or in those who have suffered a fracture.
Progression
There are four stages in the progression of frozen shoulder:
- Pre-freezing: mild symptoms
- Freezing: Painful shoulder range of motion (can last 2-9 months)
- Frozen: Less pain but range of motion becomes more limited
- Thawing: Range of motion starts getting better
The progression of the above-mentioned stages can last up to 18 months.
Symptoms
While the signs of frozen shoulder vary by individual, the most common presentations include:
- Gradual onset of pain and stiffness in the shoulder (usually insidious in onset).
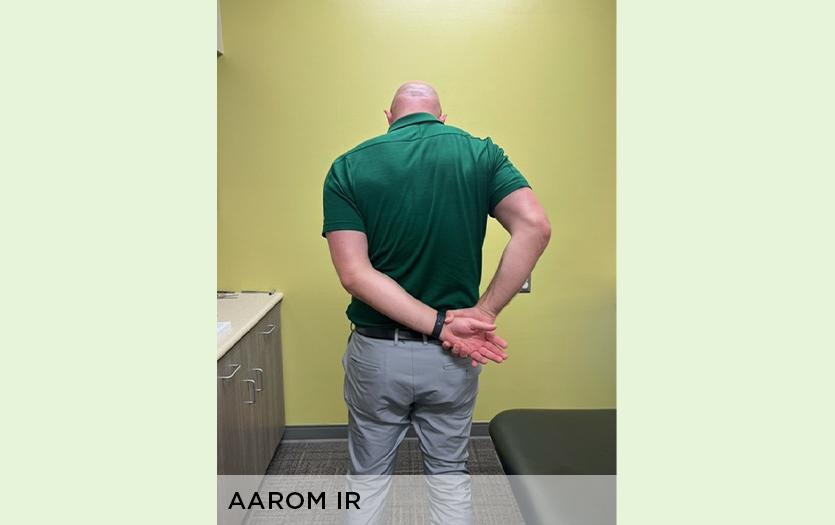
- Loss of shoulder range of motion in two or more planes (most limited in external rotation range of motion).
- Limitations in both passive (movement by the therapist) and active shoulder range of motion (moving the shoulder yourself).
Diagnosis
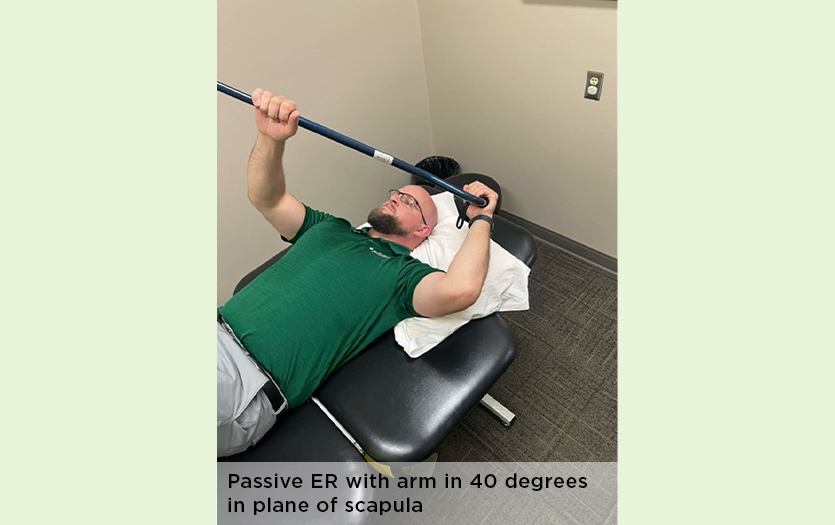
The diagnosis of frozen shoulder is based on pain and gradual loss of range of motion. When evaluating the range of motion, those with frozen shoulder typically present with the external rotation (rotating arm out) of the shoulder being most limited, followed by shoulder abduction (moving arm out to the side).
Treatment
Current evidence shows that intra-articular steroid injections along with shoulder exercises focusing on mobility/stretching are optimal for best outcomes and improvement.
Exercises should focus on stretching based on irritability levels:
- High level of irritability = short duration stretch (1-5 seconds) within pain-free range
- Moderate level of irritability = 5-15-second holds
- Low level of irritability = end-range stretching with longer duration of stretching holds

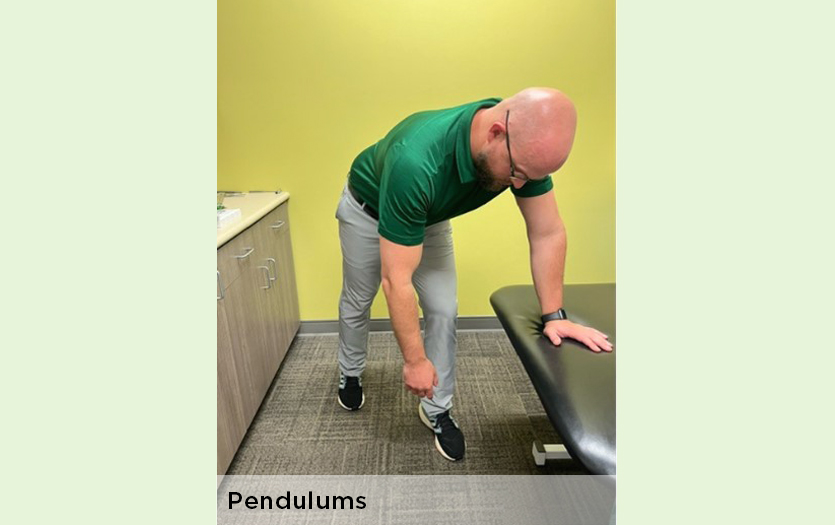
Note that aggressive stretching beyond the pain threshold in the early irritable stages can lead to less-than-optimal outcomes.
The addition of heat with stretching can assist with tissue extensibility.
Physical therapy treatment includes:
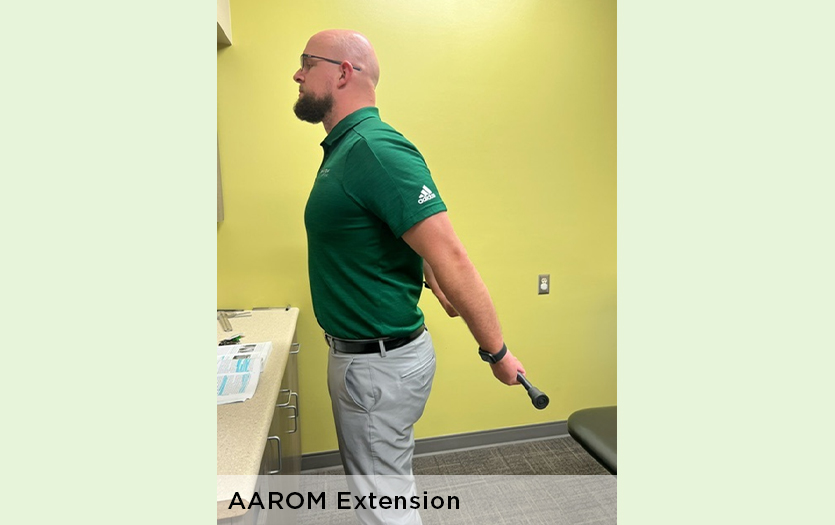
- An individualized stretching/mobility exercise prescription based on irritability level
- Manual Therapy, including joint and soft tissue mobilization
- Passive range of motion (shoulder movement performed by the physical therapist)
- Patient education on activity modification and understanding of stages/progression of the condition
Call 260-266-7400 for more information or to schedule a consultation with one of our expert physical therapists at any of our locations.
References
- Current Concepts of Orthopaedic Physical Therapy (5th Edition)
- Shoulder Pain and Mobility Deficits: Adhesive Capsulitis. Clinical Practice Guidelines
- Jospt.org



