
This post was written by Amber Glessner, NP, Parkview Vein Center.
Deep vein thrombosis (DVT) is a type of blood clot that forms in veins deep in your body. The condition is often underdiagnosed, which is why education is key. According to the Cleveland Clinic, each year, approximately 1 to 3 in every 1,000 adults develop a DVT or pulmonary embolism in the United States, making it the third most common vascular disease, behind heart attacks and strokes. While a DVT can happen to anyone, they are preventable and can be treated if discovered early.
What is Deep Vein Thrombosis?
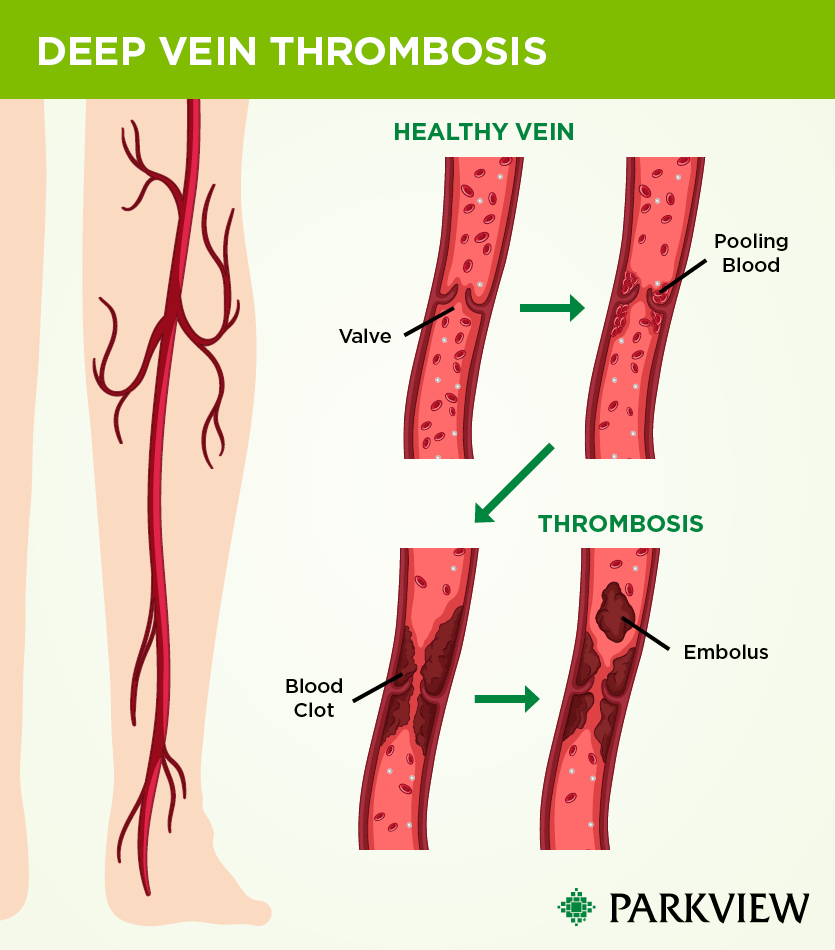
The human body has two sets of veins: deep and superficial. DVT is a condition that occurs when a blood clot (thrombus) develops within your body’s deep veins. The blood clot may partially or completely block blood flow through the vein. Most DVTs occur in the lower leg, thigh or pelvis, but they can occur in other parts of your body, including the arm, brain or other organs. The most serious complication of DVT is when the clot travels to your lungs where it becomes a pulmonary embolism (PE).
What are the risk factors for DVT?
There are different types of risk factors for DVT, from being more susceptible to getting blood clots than the general population, to having limited blood flow from some kind of immobilization.
Risks factors and underlying issues that make people’s blood more hypercoagulable (more likely to clot) include:
- Having a blood clotting disorder
- Family history of blood clots or blood clotting genetic disorders
- Having active cancer
Limited blood flow in a deep vein due to an injury, surgery, hospital stay or other type of immobilization, where your activity level has decreased, can also be a risk factor for DVT. These situations include:
- Not moving for long periods of time, such as trips in a car, truck, bus, train or airplane
- Being pregnant or having recently delivered a baby
- Being older than 40 (although a DVT can affect people of any age)
- Being overweight
- Having an autoimmune disease, like lupus
- Smoking
- Having varicose veins (blood pooling or blood being trapped in veins from the valves not working correctly can form a clot)
- Having a clot in a superficial vein, which if large enough, can travel to deep veins
- Taking birth control pills/hormone therapy
- Having a procedure to the veins where they are being accessed for IV placement (central venous catheter) or IV drug use
- Having COVID-19
Additionally, anatomy variants can cause pressure on veins and this ongoing compression can lead to a blood clot forming. Paget-Schroetter syndrome, May-Thurner syndrome and inferior vena cava abnormalities have been found after spontaneous DVT events that could not be explained except through further testing with CT scans and MRIs.
What are symptoms of DVT?
Symptoms of a DVT can include:
- Swelling of your leg or arm (sometimes suddenly), warmness to the area with red or discolored appearance
- Pain or tenderness in your leg or arm (may only happen when standing or walking)
- The veins near your skin’s surface may be larger than normal
- Symptoms that progress instead of improving
- Abdominal pain or back pain (when blood clots affect the veins deep inside your abdomen)
- Severe headache and/or seizures (when blood clots affect the veins of your brain)
Some people don’t know they have a DVT until the clot moves from their leg or arm and travels to their lung and becomes a pulmonary embolism. Symptoms of pulmonary embolism include chest pain, shortness of breath, lightheadedness, blood when coughing and fainting.
How to prevent DVT (especially if you’re high risk)
If you know you might be at a higher risk for developing a DVT, there are things you can do proactively to help prevent a clot from developing. These include:
Avoid prolonged periods of standing or sitting in one place. If you need to sit still for a long time, exercise your calf muscles. Stand up and walk at least every hour on a long flight or get out of the car every hour on long road trips.
Avoid staying in bed for long periods of time. Get out of bed and move around as soon as you can after a sickness or surgery. The sooner you move around, the less chance you have of developing a DVT.
Follow your prescription plan. Take medications as prescribed and use compression stockings after surgery if your provider prescribed them. Some surgeons will place patients on blood thinner medications after surgery to prevent clots.
Monitor varicose veins with your provider. Keep an eye on your varicose vein symptoms and talk with your provider about having them evaluated.
Wear compression stockings. If you’ve had previous clotting events, knee-high compression stockings can minimize leg pain and swelling in the future.
Avoid activities than can cause serious injury. Especially leg crushing injuries from heavy equipment, motor vehicle accidents and falls or fractures.
Keep yourself well hydrated. Especially during travel.
How is DVT diagnosed?
If it is suspected that a patient has a deep vein thrombosis, they will first receive a venous ultrasound to identify which veins have DVT in them. The presence of DVT is diagnosed by demonstrating non-compressibility of the imaged vein.
It’s also important to identify if the DVT event was provoked or unprovoked. Many times, the patient and the provider can work together to gather information and symptom timing to decide if anything correlated with the onset of the DVT event like post-surgery or long travel. A hematologist is sometimes involved as well to assist in identifying any unknown blood clotting disorders/gene mutations/protein deficiencies that the patient may not have known they had.
Treatment options for DVT
Once diagnosed, some patients may need to be treated in the hospital, while others may be able to have outpatient treatment, depending on how extensive the clot is and how their symptoms are affecting them.
Common treatments for DVT include medications called anticoagulants (also known as blood thinners), compression stockings and elevating your affected leg(s).
The main goals of treatments are to:
- Keep the clot from getting bigger and involving other veins
- Prevent the clot from breaking off in the vein and moving to the lungs
- Lessen the risk of another blood clot
- Prevent long-term complications from the blood clot (like chronic venous insufficiency & post-thrombotic syndrome)
Anticoagulant medications make it harder for your blood to clot and can be administered as a pill or an injection. They also stop clots from getting bigger and prevent blood clots from moving. However, anticoagulants don’t destroy or make every blood clot disappear. When clots don’t fully go away, they shrink can become like “scars” inside your veins called old clots or chronic clots. Old clots may result in long-term leg swelling.
Anticoagulants are sometimes prescribed for only a few months (usually 3-6 months) or may need to be taken indefinitely. Treatment time differs depending on the specific situation of each patient. Factors that are considered for length of treatment include if you’ve had clots before or if you are being treated for another illness like cancer or an autoimmune disease.
If you can’t take anticoagulants due to active bleeding or a high risk of bleeding, or if you have blood clots while taking blood thinners without missing doses, then your physician may have to perform a procedure to insert an inferior vena cava (IVC) filter as treatment. This procedure is done under local anesthesia. The physician will insert the IVC filter through a catheter into a large vein in your groin or neck and then into your vena cava (the largest vein in your body). Then, if blood clots in the veins break off and travel, the IVC filter is designed to prevent large blood clots from reaching your lungs and causing a pulmonary embolism. While and IVC filter helps to prevent a pulmonary embolism, it doesn’t keep more blood clots from forming in your veins.
In a minority of cases, when the DVT is extensive, invasive treatments such as catheter-based procedures, may be required. These steps are usually taken in cases where the clot burden and pain are so extensive that the patient has trouble walking and getting around. Then the clot can be removed from the vessel.
What is post-thrombotic syndrome?
Post-thrombotic syndrome refers to symptoms and signs of chronic venous insufficiency that develop following DVT and is a common, burdensome and costly complication. Symptoms and signs of post-thrombotic syndrome may include:
- Leg pain
- Leg heaviness
- Chronic edema (lymphedema)
- Skin pigmentation changes (darker lower legs)
- Venous ulcers
With this complication, the clot causes the vein valves to work harder, forcing blood up and around the clot above it. This is much like a boulder in the road, and it can damage the vein valves permanently as they work hard under pressure to move blood around the clot. The vein valves are built to work in one direction pushing blood up. When the vein valves are damaged, they do not close properly and reflux. Some blood is properly going up, but some blood is also going the wrong way or refluxing in the lower leg. Reflux of the vein valves allows blood to pool in the veins causing pressure to build over time (venous hypertension).
When to call a doctor
It’s important to call your doctor right away or go to the emergency room if you have symptoms of a DVT. Don’t wait to see if your symptoms go away. Get treatment immediately to prevent serious complications.



