
This post was written by Allison Clemens, PharmD, Parkview Health.
While it may not be marked on your calendars, November is National Diabetes Awareness Month. Many Americans, if they are not impacted by the condition personally, know someone who is affected by diabetes. According to the Centers for Disease Control and Prevention (CDC), 10.5% of the total adult population have the disease which, when uncontrolled, can lead to irreversible damage to a person’s body. Thankfully, there are simple techniques that can help minimize these risks and support a healthy lifestyle.
Strategy No. 1: blood-glucose testing
If you have been diagnosed with diabetes, you probably have been instructed by your physician to complete daily blood glucose (sugar) readings. This is an effective tool for measuring if your blood sugar levels are within a healthy range.
What’s the best way to test my blood sugar?
There are different methods and tools that can be used to test your blood glucose. Continuous monitoring systems allow for around-the-clock monitoring of your blood glucose levels without having to poke your fingers multiple times a day. Traditional lancets, lancing devices, and blood glucose monitors work well if a person only needs to know blood glucose levels a couple of times a day. It's best to discuss what type of testing is best for you with your physician.
I test my sugar, but I don’t know what a good or bad number is?
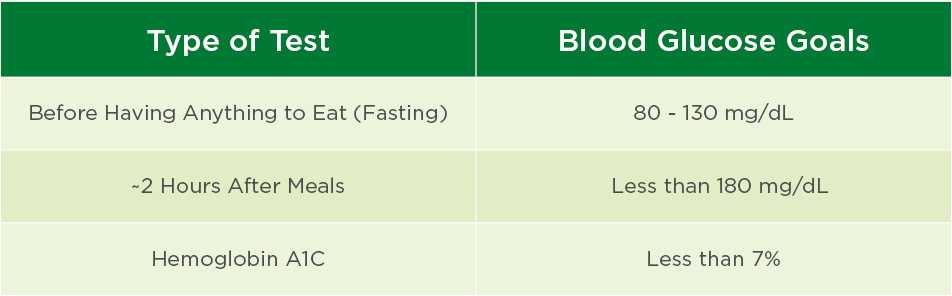
Depending on when you tested your blood glucose, the target range is different. Your blood glucose goals may also be different based on your age, type or severity of diabetes, and overall health. Always confirm your individual hemoglobin A1C and blood glucose goals with your healthcare provider.
Hemoglobin A1C is a specific type of test that gives you a summary of your average blood sugars over the past 3 months. This takes a special type of machine that can be purchased over the counter at some pharmacies or done in a hospital laboratory. You can test your blood sugar routinely at home with a lancing device and blood glucose monitor.
I tested my blood sugar like I was supposed to, what do I do now?
It’s important to ensure that you are writing down all your results in a small journal or notebook categorized by the date and time of day when you tested your blood sugar. This helps you keep track of trends and gives your healthcare provider a better picture of your blood sugar control. If you notice that your results are consistently above or very below your blood glucose goal, let your provider know as a medication intervention may be needed.
Strategy No. 2: lifestyle changes
While medications are the cornerstone of treating diabetes, you can impact the management of this chronic disease by utilizing non-medication interventions.
What else can I try or do to maintain my health when living with diabetes?
We have all been told about the importance of having a healthy diet and exercising regularly, but implementing these concepts with our busy lives can be difficult. If something is worth doing, it’s better to do 25% of that activity than nothing at all. This concept certainly applies when it comes to incorporating diet changes and exercise into your life. A great place to start when looking for information about diet is nutrition.gov or the “Nutrition and Recipes” section of our blog.
You don’t have to get a gym membership to become active, either. You can find more information on how to casually become more active by visiting the U.S. Department of Health & Human Services website and searching “exercise,” searching for helpful videos online or just going for a walk. The hhs.gov site also has the most recent “Physical Activity Guide for Americans.” These show that it’s recommended that people get 30 minutes of moderate exercise five times a week. While this is an excellent goal, start with small changes that work for your lifestyle and increase over time.
Strategy No. 3: monitoring complications
Maintaining a healthy lifestyle, and taking your medications on time is very important, but it’s also critical to know when you may be having complications due to diabetes.
What complications should I be looking for?
Due to the nature of the disease, diabetes can damage blood vessels and nerves within the body. This results in reduced blood flow throughout the body and can lead to a lack of feeling in extremities like your eyes, feet or hands.
Feet: Visually inspect both feet daily to look for any abnormal sores, redness, inflamed areas or discoloration.
Eyes: Vision loss can progress slowly and not be obvious at first. Potential red flags include development of impaired color vision, empty areas in your visual field, or spots/dark objects floating in your visual field. It’s recommended to have a yearly eye examination to check for any loss of vision.
Neuropathy: Keep track of any instances when you experience a new or worsening loss of feeling in your feet or hands. You may notice tingling, numbness, burning or feel something similar to the sensation when a body part “falls asleep.”
Let your physician know if you notice any changes in the areas mentioned above!
Early detection and effective management of diabetes helps to prevent or slow down potential consequences of this chronic disease. Implementing any of these tips can lead to an overall improvement in your health and help you manage your diabetes.



