
This post was written by Courtney Leach, social media manager, Parkview Health.
I can admit it now, I wasn’t thrilled when I learned we would be meeting at Parkview LaGrange at 6:45 in the morning. But cruising up State Road 3, “Kodachrome” by Paul Simon coming through the speakers, it was a bit of a treat to greet the day. As the miles elapsed from the app on my dashboard, I saw ominous dark clouds to the west and a blazing coral wave bleeding up over the tree line to the east. I was somewhere in between, where the two skies met and mingled.
I caught the first light stretching out over Sylvan Lake. I passed turkey buzzards picking at breakfast and shaky spring foals skipping in their dewy pastures. I snaked along, by mammoth overhead sprinklers spanning across primed fields, tractors dozing here and there, waiting to see which side of the sky would win and dictate their workday.
The phased approach
I met Shea Pyle, BS, ACSM EP-C, an exercise physiologist, on the farthest end of the parking lot, near the entrance for Outpatient Therapy. We walked down the steps to a door on the lower level. A left at the cafeteria and we arrived at the Cardiac and Pulmonary Rehab room. This is Shea’s space, where he helps patients recoup and reclaim their physical stamina and self-esteem.
After we exchanged a few pleasantries, just before 7 a.m., the first gentleman of the day walked in. He was in Phase 2 of Cardiac Rehab. Shea explained that there are three phases to the cardiac rehabilitation process.

Since assuming the role of manager for Cardiac Rehab in Allen County, Emily Keltner has worked diligently to improve the referral process for Parkview Heart Institute (PHI) patients. During Phase 1, Cardiac Rehab staff (primarily exercise physiologists, like Shea) visit patients in the hospital who qualify for Cardiac Rehab. They educate them on what is involved in the Phase 2 program, the benefits of going, provide educational material that will be covered during their Phase 2 onboarding and answer any questions they have. They ask which location the patient prefers and put that information into the medical record system so that location can call them to schedule the orientation appointment for Phase 2.
“We used to wait until they’d had their follow-up appointment with their cardiologist,” Shea explained. “But now the care team can clear them for exercise when they get discharged from the hospital if they think it’s safe. This has helped us get people in much quicker and eliminate lost time.”
Phase 2 involves 36 sessions of exercise while attached to a heart rate monitor and supervised by a Cardiac Rehab team member. Sessions for Phase 2 patients involve arm and leg exercises, increased gradually over time, for 30-60 minutes. “You see a big demeanor shift over the course of their 36 sessions,” Shea said. “That first appointment, they’re so scared. They’ve just had a life-changing event and they’re terrified it will happen again if they push their bodies. So much of the first few appointments are about gaining the confidence to move again.”

Shea watches the heart rates for all Phase 2 patients on his computer monitor, and routinely checks in with them both verbally and by taking their blood pressure during activity. “In order to take this job, I had to be very comfortable reading the heart rhythms.” He is looking for any concerning changes or patterns, at which point he would intervene. Parkview LaGrange has PPG cardiologists on staff Mondays and Wednesdays. Shea defers to the ER physician in charge on other days. “We have a standard protocol for addressing medical emergencies and I have a lot of support here, if I need help. Mostly, when we do have complications, it’s a patient’s blood pressure dropping or they become light-headed, so I have them sit and rest for a bit.”
Phase 3 is for those who wish to pay a small monthly fee for continued use of the equipment in the facility. This is a safe, but more independent option for Cardiac Rehab grads. For residents in LaGrange, entering Phase 3 is a great option, as there are limited choices for gyms in the area.
“Friday’s the big day!” Shea said to his 7 a.m. appointment, as the gentleman peeled the stickers off of the backs of the electrodes he’d attach to his chest. “Session 36. You made it.” Shea then began the series of check-in questions he offered each of the patients as they arrived, “Did you get in any exercise yesterday? How’s your sugar?” After reporting their recent activity, the patients would weigh in and Shea would check their blood pressure. Then it was time to get moving.
Shea tailors each patient’s exercise routine to their abilities and condition. If they are experiencing knee or shoulder discomfort, he’ll work around those sore spots to keep them comfortable. Before they ever touch a machine, he has a one-on-one orientation to cover education (Mary Buuck, RN, assists with Pulmonary patients), goals and the equipment. Patients also do a 6-minute walking test. “I want to understand where they are, physically and mentally.”
A twenty-something takes on a challenge
Men have gathered for centuries, around fires, bar stools and locker room benches. While the motive is to mend their stamina and moxie, make no mistake, when local guys convene in the rehab room in LaGrange, it’s akin to a modern golf course clubhouse. Shouting output numbers over their shoulders as both a cheer and a challenge, comparisons, friendly jabs … at various points in the day it was the hospital equivalent of a pickup basketball game at the neighborhood park, egos and tenacity rebounding before our eyes.
The healthy competition doesn’t bother Shea a bit. “It can certainly push them,” he said. “Which can be a good thing. A lot of times, patients think they’re getting in plenty of movement, but then they come in here and see the monitors and realize they haven’t really been elevating their heart rate as much as they thought outside of the gym. There’s a difference between yard work and what we’re doing with these machines.”
The ease with which these patients engaged in playful one-upping is evidence of the inevitable intimacy fostered in smaller towns. “It’s fun to hear them sharing these stats and giving each other a hard time. Most of these guys have known each other for years. It’s part of what’s so special about LaGrange. You wouldn’t get this at the bigger locations.”
It’s a particular charisma that the exercise specialist is very familiar with. LaGrange bears many similarities to Berne, Indiana, where Shea grew up. “As a teen, I always loved working out. I played four sports and, eventually realized it was the exercise I enjoyed more than the actual games.” In 2017, during his final semester at Ball State University he began an internship in Cardiac Rehab at the Parkview Heart Institute. He spent time shadowing in the Heart Station and took an EKG class. Shea graduated with a degree in Exercise Science in the spring of 2017, but there were no openings in Cardiac Rehab, so he took a job with Parkview’s Wellness team, doing community health screenings.
After a team member took another position, a job became available in the brand-new Cardiac Rehab gym at Parkview LaGrange. So, in July 2018, at just 23 years old, Shea welcomed the first patient to the community hospital facility and became the primary team member overseeing the program.
A slow start, unexpected stop, and restart
“Initially, I was basically cold calling patients trying to get them in here,” Shea recalled. Eventually, he got up to 12-14 patients three times a week. Then COVID hit.
In late March 2020, Cardiac Rehab followed on the heels of Physical Therapy (and many other departments) and closed down sessions as the health system fought to address the new and unsettling pandemic. “Things were changing every day. After we closed, I became a greeter in the Emergency Room. I would write down the names of everyone who came into the hospital and their temperature. I was never scared, but I knew it would impact our patients. We reopened, with new safety and cleaning protocols, in May 2020, and we’re just now getting back to the same patient volume we had before the pandemic.”
If you forget about COVID even for a second, you need only watch Shea dutifully distributing sanitizing wipes for the equipment. In addition to an increased demand for cleaning supplies, the pandemic also introduced a new patient population – those impacted by the lasting effects of coronavirus. A patient can be referred by their physician if they are having a hard time breathing or maintaining their oxygen level post-COVID. “I’m seeing pretty good success with these patients,” Shea said. “Every COVID story is a little different, but we find that once we get them in here and start building up their endurance, they get some of that confidence back and make strong progress fairly quickly.” Shea has his own COVID story. He contracted the virus in December 2020, losing 30 pounds and his sense of taste and smell.
“It’s OK to get winded”
While some of Shea’s post-COVID patients are a bit younger, the majority of his day is spent with older adults and, I couldn’t help but notice, predominantly men. During a brief break in activity, I asked Shea about the demographics on his docket for the day. “It ebbs and flows, but I would say I do see more male patients overall. The gap is closing, but it’s still more common for men to have heart events. It seems like women are busier, or maybe more concerned with taking care of others, so they are less likely to participate.” Adherence is a real problem for Cardiac and Pulmonary Rehab patients, which is surprising, considering finishing the program can decrease your risk of recurrence by up to 35%.
.jpg)
Around 9 o’clock, things really started to pick up. A mix of Phase 3 gym goers and Phase 2 patients kept Shea busy. Between check-ins, helping with machines, watching rhythms and oxygen levels, and “running the floor” (checking blood pressures during activity), he was in a state of perpetual motion; a one-man band, entirely present, keeping all of the necessary plates spinning.
I held a position by the water cooler and listened in as the friends and fellow patients joked about their golf games and meeting for coffee at the local McDonald’s. I asked one gentleman how long he’d been coming. He’d been in Phase 3 for more than a year. “I like the atmosphere,” he said, “And Shea does a good job.” Another chimed in, “It’s like babysitting!” he joked. “Yes, he’s a great babysitter,” the first gentleman agreed, subtly tipping his cup up toward Shea.
From my spot near Shea’s desk, it was hard to ignore the, at-times, heavy huffing and puffing. “It’s OK if they’re winded, as long as they can carry on a conversation,” Shea assured me. “Plus, I get to know their normal and I can tell if something is different or concerning. Sometimes, pulmonary patients in particular, start talking and forget to breathe.” He asked a few patients to stop and rest when their numbers climbed to a range he didn’t like.
The goal for Cardiac Rehab patients – many of whom are post-surgery or recovering from a major heart event or diagnosis – is to get their heart rate into the target range and maintain it. Then for it to come back down. For Pulmonary Rehab patients, most of whom have COPD or are post-COVID, the goal is to maintain their oxygen level above 88%. “The challenging thing with Pulmonary patients is that they are often dealing with a chronic diagnosis. This isn’t going to be cured, we’re just trying to manage it. That can be tough mentally.”
When someone is feeling down or hesitant, Shea defaults to subtle but sincere encouragement.
“Nice!” “Great work!” “Dang! You’re feeling good today!”
“My grandfather died of a heart attack my senior year of high school and that certainly makes it more personal for me. These are people who are used to doing whatever they want. Suddenly, they’re feeling limited and like they’ve lost their independence. They’re facing unknowns. I don’t treat them like they’re fragile. I’m not going to push them to a point where they aren’t safe, but I want to help them get their confidence back and see that this isn’t what life has to be like. They can return to where they were and improve beyond that.”

Over the course of a few hours, the door swung open and closed a handful of times and, as more patients attached their monitors, checked in and got to work, the volume rose in a roaring ensemble of energy. The beeping of monitors, the clicking of seats sliding into place, the pumping of recumbent pedals, the whishing of the airbike, the uneven thud of sneaker soles alternating on the rubber pad of the treadmill and the constant cranking of the hand levers. It was easy to get lost in the sonic sum of the room’s moving parts.
A person about the people
If the machines weren’t humming, it was fairly common for some healthy water cooler conversation to break out. Patients exchanged war stories of stents and surgeries. Pacemakers, clots and blockages. But it wasn’t all about their medical misfortunes. They talked about travel, relationships (an upcoming 50th anniversary!), crop conditions and challenges, the weather, glory days on the football and softball fields, and, yes, politics. In the span of an hour, they could solve all the world’s problems.
“There’s typically at least one patient who hangs out and talks,” Shea said. “I love hearing all their stories, and it keeps the mood light.” The socialization is as much a form of medicine as the movement is. After all, the group has a shared experience: A second lease on life.
Of course, it’s inevitable that some patients just stand out. “I had a 93-year-old woman who came in and said, ‘I guess I’ll try it.’ And she made it all 36 sessions and did Phase 3 for over a year. She quit coming during COVID, but she still sends me cards at Christmas and Valentine’s Day.“
When I asked him about the responsibility of overseeing the program at LaGrange, Shea was quick to drop names. “There are so many people who helped me and continue to help me in this job. Cale Tabler, Jim Uecker, Nickole Kosan, Nicole Schaekel, and Megan Zink have been so incredible. I spent a lot of time observing Kim Clouse, who oversees the program at Noble, because it’s a similar size. I watched how she ran things and I still reach out to her when I have questions about pulmonary patients, since she’s a respiratory therapist. And Trevor Fry, RN, the ER manager here is an amazing resource. He’s just awesome to work with.”
All of the Cardiac and Pulmonary Rehab programs at our community hospitals are run by either an exercise physiologist, registered nurse or respiratory therapist. Parkview Regional Medical Center has all on staff.
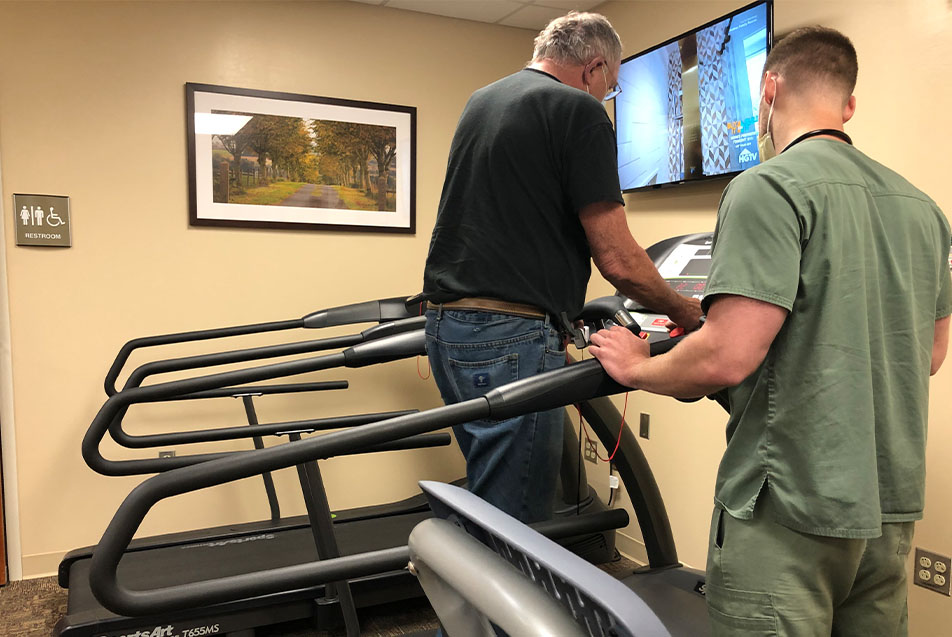
One of Shea’s final patients of the day was there for Supervised Exercise Therapy (SET), a treatment he has offered since February 2021. SET is designed to help those experiencing leg pain as a result of restricted blood flow. This being only his second SET patient, Shea admits, “I’m learning right along with him.” The treatment is predominantly treadmill-based. Patients walk at a prescribed pace and incline, checking in when they reach different degrees of discomfort, until they reach a “5”, the highest on the pain rating scale, and stop until they can go again. The benefits are both mental, because it helps patients get used to feeling the pain and pushing past it, and physical, as the practice increases blood flow. Participants also begin taking a vasodilator (medication that opens blood vessels) at the start of treatment. Just seven visits in, the patient was already feeling improvements. Notably, it was easier for him to get up off the ground when working in his garden.
“When I hear them talk about how well they’re doing at home, it makes me feel like my work matters. I’m helping people. It’s the type of environment I always imagined myself in. Maybe not this demographic necessarily, but I love it so much. I know how lucky I am to have this opportunity at my age. These are the jobs that you take and never leave. I’m proud of what I’m doing here.”
I thanked Shea for letting me look over his shoulder and walked out into the gentle rain shower patients had been commenting on all day. There was the unmistakable clip-clop of hooves in the distance. One buggy coming and one going.
LaGrange, like many of the smaller communities we serve, has a distinct personality, punctuated by particular characteristics. After spending time with Shea, in his gym with its chorus of whishing and walking and conversation, the attributes that stood out to me above the rest were the connections and encouragement. The space I stepped into was one where neighbors quipped about unmanaged weeds and fellow survivors spurred each other on, toward goals and a capacity once, in the not-so-distant past, feared lost.
And then there’s Shea. The captain of a concerted climate, designed to introduce the beautiful possibility that this isn’t over. That setbacks are different than swan songs. That progress is always possible with hard work and a few drops of grit.
Shea keeps showing up for his patients and urging them to keep showing up for themselves. All things heal, but not without time and humility. As I witnessed firsthand in LaGrange, you just have to have the right attitude. You have to have someone gifted in the art of the subtle nudge. And above all else, you have to have heart.



