This post was written by Atiya Khan, MD, PPG – Pediatric Neurology.
In the United States, there are 3.5 million people who have active epilepsy. Out of that, 15% have recurrent seizures. Additionally, about 5% of epileptics suffer from seizure clusters (in which the individual has several seizures in a row or has recurrent seizures within hours) or status seizures (lasting a long time).
This is important to know, because once someone has a seizure, often they end up going to the Emergency Room, hospitalized or with serious injuries like fractures. For individuals with uncontrolled seizures, the risk of dying is three times that of people whose seizures are controlled.
In surveys, approximately 75% of adult patients with epilepsy say that their biggest fear is that they don’t know when a seizure is coming. The disease is unpredictable. They could be crossing the road, in the bathroom, sleeping or eating in a restaurant.
In another survey, 80% of patients and caregivers said they don’t have a rescue medication, meaning that once a seizure begins, they are unable to intervene. At least 30% of adults and 40% of adult caregivers reported that they had to go to the ER for intervention for recurrent seizures. From the time someone calls an EMS to the time they reach the ER, the time on average is 42 minutes. From the onset of seizure to intervention by a medical professional, the average time is 56 minutes.
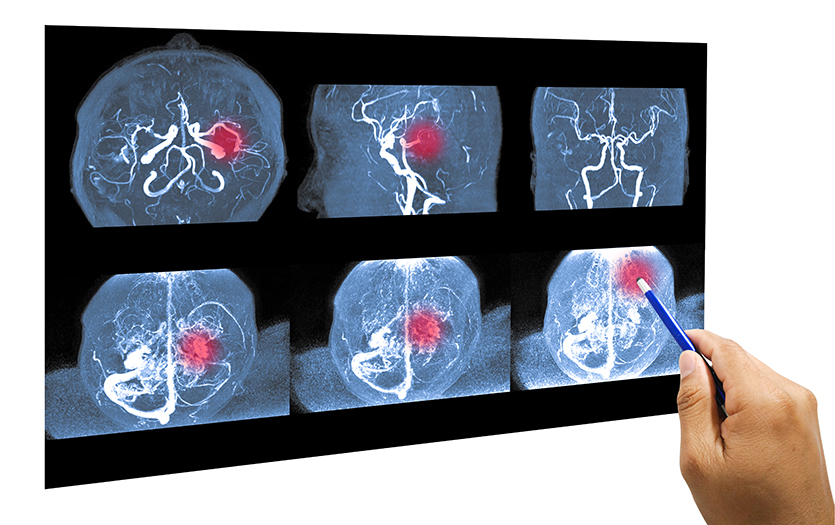
If seizures are not treated early, it becomes harder and harder for the individual to come out of it. If a seizure doesn’t stop within 15 minutes, we call that being in status. Some epileptic patients could seize for hours. That’s a long time to be seizing. If treatment is delayed, it can result in more negative outcomes, such as the need for a ventilator, injuries or brain damage and death.
This is why rescue medication is so important for patients who have seizures, but particularly those who are prone to status or cluster seizures. Patients who have cluster or status seizures are 30% more likely to have head trauma, dental injury or fracture. With seizure clusters they have a 73% chance of an ER visit and/or hospitalization.
Medications for emergency intervention
For years, the only FDA-approved medication available to the public to treat seizures has been DIASTAT® (diazepam rectal gel). While this medication is highly effective, it does present some social and logistical issues. The medication has to be administered via a suppository inserted into the anus. For older children and teenagers, this can cause some anxiety. Additionally, many schools either don’t have a school nurse or they share one with other buildings. This puts a lot of pressure on teachers to learn how to administer the medication. It also brings up a number of concerning scenarios regarding other students in the class.
Oral medications have historically presented risks as the individual could choke or aspirate. An unconscious patient cannot actively swallow. These limitations have left families, caregivers and patients frustrated and anxious for years.
Exciting developments
Thankfully, over the past year, two new medications have been approved to offer epileptics new options for seizure control.
The first is Nayzilam (Midazolam nasal spray). This is approved for children 12 years and older. This can be given very easily as a spray into the nose. It is a very small volume (0.1 ml) and the rescue medication gets absorbed into the bloodstream from the nasal mucosa. This nose spray can be administered again into the other nostril if the seizure hasn’t stopped within 10 minutes. It is safe to use while a patient is actively seizing or unconscious. Potential side effects are sedation and nasal irritation.
The second drug is VALTOCO® (diazepam nasal spray). This spray deposits Diazepam into one nostril and is absorbed from the mucosa so there is no risk of aspirating. This is approved for patients six years or older and comes as blister packs with appropriate dosing for the patient’s body weight. Caregivers can administer the spray while the patient is experiencing an active seizure and can be repeated, as needed, within four hours. The potential side effects are mild, and include sleepiness, nasal irritation and a strange taste.
Children under 6 will still need to utilize DIASTAT® for seizure intervention.
As with any medication, there are things to be cautious of. Be aware of any potential drug interactions and never combine these medications with other sedatives, such as opioids or alcohol.
Forming an action plan
Nearly 70% of adults with epilepsy do not have a seizure action plan. This document would outline when and how to intervene, when to seek emergency care, etc. In pediatrics, that number is far less because most schools require one, but there is no mandate for adults.
Now that we have more options, it’s more important than ever to form a seizure action plan. Talk to your neurologist or pediatrician about these new medications and the best course of treatment should your child experience a seizure event.
The Epilepsy Foundation has so many great resources, including printable action plan templates. Simply download and print one and fill it out with your physician or care team.
Additionally, they offer seizure diaries and seizure first aid guidance to include with the care plan.
Given the size of these new nasal sprays, it would be convenient to keep one at home, one at school and one at the babysitter’s, or anywhere the patient spends a lot of time. The size of these nasal sprays makes it easy to carry. That way, when you need it, it’s there.
I would also encourage caregivers to take advantage of test kits which would allow them to practice in a calm manner how to give these nasal sprays. One of the biggest hurdles to intervention is panic. When someone begins seizing, the person with them freezes. The more you can practice administering the nasal spray or medication, the more prepared you will be to help when it matters most.
Talk with your provider and explore whether these medications would be right for you or your child. It’s important to be aggressive in your treatment plan and find the best rescue medications for your situation.