This post was written based on a presentation by Alexander Robitaille, DO, FAAPMR, Ross Nelson, PT, DPT, CSRS, CBIS, NCS, and Justin Shaffer, PT, DPT, CSRS.
Every 40 seconds, someone in the United States has a stroke. These health events are a leading cause of long-term disability in our country, so it’s important to understand the options and outcomes associated with recovery.
Post-stroke recovery considerations
When a person comes into the hospital after a stroke, they often need rehabilitation to safely return home. This can lead to uncertainty around the level of rehabilitative care that will produce the best outcome. Patients and their loved ones work with their care team to consider whether a skilled nursing facility, inpatient rehabilitation facility, outpatient therapy or home health care will meet their needs.
Inpatient rehabilitation, which specifically aims to rehabilitate individuals with neurological deficits including but not limited to stroke, offers key benefits, including:
Time – Inpatient rehab requires at least 3 hours of therapy, 5 to 7 days a week. This is a much higher intensity of rehabilitation than many skilled nursing facilities that offer 1-1.5 hours of therapy a day, 3-5 days per week.
Specialized staff – The staff in an inpatient rehabilitation unit often consists of physiatrists specialized in rehab medicine and addressing concerns unique to neurologic conditions such as stroke. These issues may include spasticity or an increase in tone after stroke, bowel and bladder dysfunction, and alertness impacted by stroke. This team also includes physical, occupational, and speech therapists who often specialize in stroke rehabilitation and nurses, who specialize in rehab nursing.
At Parkview Inpatient Rehabilitation, we have three occupational therapists, two physical therapists who are Stroke Rehabilitation Specialists, as well as two Board-Certified Neurologic Clinical Specialists for physical therapy. We also have Certified Rehab Registered Nurses to care for patients at Parkview.
Sophisticated resources –The Parkview Inpatient Rehabilitation program has continued to grow in staffing, rooms, resources, and programming. The therapy team has progressively begun instituting high-intensity gait training and other high-intensity exercise programming to assist in stroke recovery. The research has continued to show that patients who receive high-intensity gait training as the primary intervention after a stroke have better outcomes than those who receive general standing and sitting balance activities.
Fear around high-intensity exercise and health events
The old mindset of the medical community centered around concern that mobilizing or introducing exercise to patients following a stroke would result in an increased risk for cardiac events, additional stroke, syncope or even death. Many of the initial studies around the safety of this population focused on cardiac patients and overwhelmingly supported that exercise is safe for these individuals. In an article featured by Cochrane Library, titled “Bedrest for Uncomplicated Myocardial Infarction,” the authors share that there is not a large difference between short or long periods of bedrest when considering adverse events, supporting early mobilization.
A 2006 study (Pavy) followed 25,420 French cardiac rehab patients and found only 20 cardiac events occurred, none of them fatal. This totaled to about 1 event per 49,565 hours of training. In 2018, researchers (Wewage) conducted a systematic review using 23 studies where participants engaged in high-intensity interval training (HIIT) (classified as >85% HRmax, RPE >15). Based on more than 31,000 training sessions and 22,000 hours of activity, their findings revealed only 7 adverse events, including 1 major but nonfatal cardiac event and 1 minor cardiac event, with 5 others related to orthopedic conditions or anxiety.
What does this mean for stroke survivors?
The majority of stroke survivors (about 75%) have coexisting cardiac disease. Without enough evidence for this specific population, experts recommend stroke survivors follow the same guidelines used for individuals recovering from a myocardial infarction. Specifically for high-intensity gait training, current recommendations support that stroke patients exercise at 70-85% of their age-predicted heart rate maximum to maximize recovery while also maintaining safe exercise parameters.
Principles of neuroplasticity and motor learning
Best clinical practice stroke rehabilitation focuses on principles of neuroplasticity. The National Institutes of Health (NIH) defines neuroplasticity as “the ability of the nervous system to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections.” Simply speaking, neuroplasticity is our brain’s capacity to change, adapt, and learn new skills, memories, etc. This is vital in stroke rehab as the interruption to alter physical strength and mobility is not in our muscles but in our brains.
Therapists adhere to 10 principles of neuroplasticity to best affect the brain and induce positive change. Three principles—specificity, repetition and intensity—are specific to high-intensity gait training and a focus of Parkview’s stroke recovery work.
Specificity states we need to do the task we want to do to improve it; walk to improve walking.
Repetition highlights the more opportunities we perform walking, the more opportunities the brain has for neuron communication and then connection.
Intensity matters, because as we engage patients in exercise at 70-85% of age-predicted heart rate max, we see increased opportunities for neuroplasticity. Specifically, when exercising at these intensities, there is an increase in nerve growth factor, one of which is called Brain-Derived Neurotrophic Factor (BDNF), which helps to facilitate neuronal connectivity, allowing for greater gains toward the ultimate goal of improving function and walking.
The role of gait training in stroke recovery
At Parkview’s Inpatient Rehabilitation Unit, the physical therapy team has increased training and emphasis on high-intensity gait training as a key pillar in our treatment strategies and programming for stroke recovery. Physical therapy staff has been trained and equipped to perform high-intensity gait training sessions with heart rate monitors to maintain safe exercise parameters and work towards achieving the recommended heart rate ranges to induce neurological recovery.
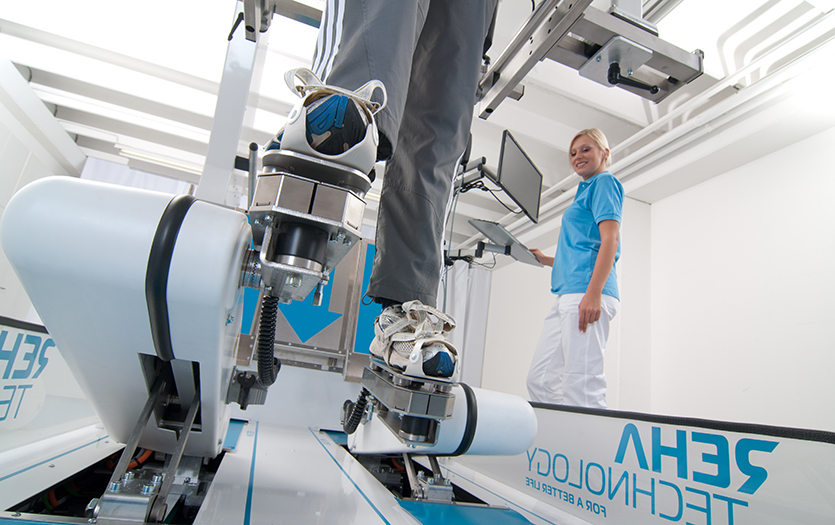
The unit continues to increase options for these devices, such as harnesses to provide body weight support during gait training. This allows earlier mobilization of stroke survivors with a wide range of physical abilities in a safe way for patients and therapists. Early mobilization is vital for recovery and increasingly promoted and possible.
As patients progress in gait, continued challenge is applied to increase heart rate response into target ranges and to facilitate the principles of neuroplasticity. To augment the challenge required to meet the demand for recovery, therapists may create challenges by altering the velocity of gait, resistance for propulsion and limb advancement, adding inclines or stairs, or challenging through multi-directional stepping.
High-intensity gait training has been shown to be effective in acute, sub-acute and chronic stroke populations. When provided by skilled staff with appropriate monitoring, this method is both safe and desirable for increased opportunities for neural connectivity, learning, and, thus, recovery. Many stroke survivors have seen excellent recovery in their walking from the growing understanding, use and adherence to high-intensity gait training principles, and we only see this trend growing as more information and research becomes available.
To learn more about Parkview’s stroke program and other Inpatient Rehab offerings, visit us here. For additional stroke support information, see what Parkview has available here.
References
Lennon S, et al. Gait outcome in outpatient physiotherapy based on the Bobath concept in people post stroke. Disability and Rehabilitation. 2006; 28(13-14): 873-881.
Dobkin B, et al. Should Body Weight-Supported Treadmill Training and Robotic-Assistive Steppers for Locomotor Training Trot Back to the Starting Gate? Neurorehabil Neural Repair. 2012; 26(4): 308- 317.
Hornby TG, et al. Enhanced Gait-Related Improvements After Therapist- Versus Robotic-Assisted Locomotor Training in Subjects with Chronic Stroke: A Randomized Controlled Study. Stroke. 2008; 39(6): 1786-1792.
Hornby TG, et al. Contributions of Stepping Intensity and Variability to Mobility in Individuals Poststroke: A Randomized Clinical Trial. Stroke. 2019; 50(9): 2492-2499.
Holleran CL, et al. Feasibility and Potential Efficacy of High-Intensity Stepping Training in Variable Contexts in Subacute and Chronic Stroke. Neurorehabilitation and Neural Repair. 2014; 28(7): 643- 651.
Leech KA, et al. Effects of Locomotor Exercise Intensity on Gait Performance in Individuals With Incomplete Spinal Cord Injury. Physical Therapy Journal. 2016; 96(12): 1919- 1929.
Ardestani MM, et al. Compensation or Recovery? Altered Kinetics and Neuromuscular Synergies Following High-Intensity Stepping Training Poststroke. Neurorehabilitation and Neural Repair. 2019; 33(1): 47-58.
Ardestani MM, et al. Kinematic and Neuromuscular Adaptations in Incomplete Spinal Cord Injury after High- versus Low-Intensity Locomotor Training. Journal of Neurotrauma. 2019; 36: 2036-2044
Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the AHA Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007
Physical Activity and Exercise Recommendations for Stroke Survivors: A statement for healthcare professionals from the AHA/ASA. Stroke. August 2014.
Pavy B. Safety of exercise training for cardiac patients: results of the French registry of complications during cardiac rehabilitation. JAMA Internal Medicine 2006
Rognmo O, Moholdt T, Bakken H, Hole T, et al. Cardiovascular risk of high- versus moderate- intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126:1436– 1440
Wewege, M. High-Intensity Interval Training for Patients with Cardiovascular Disease – Is It Safe? A Systematic Review. 2018.
Physical Activity and Exercise Recommendations for Stroke Survivors: A statement for healthcare professionals from the AHA/ASA. Stroke. August 2014.



