This post was written by Courtney Leach, digital/social media manager, Parkview Health.
As a support team member gifted the opportunity to observe many of the unique arms of the health system, I have seen firsthand the powerful results of personalized care. I’ve learned that two expert minds working together are better than one. And that, in almost every instance, that’s only amplified the broader we make the circle of knowledge and resources around the patient. Through sacred moments and conversations, I’ve seen that every loss or unforeseen setback brings grief. And that they give way to new life and growth, too.
While looking over the shoulders of our dedicated team members doesn’t make me an authority on healing, it has given me a unique perspective on the ingredients typically required for overcoming a health event–the common threads in almost all of the testimonials that inspire.
First and foremost, the individual has to be willing to put in the work and fight for what they want. (See also: determination; grit.) They have to be open to empathy, both the giving and receiving of it. They often have a sense of curiosity and aren’t afraid to ask questions. And of course, they never lose hope.
I was fortunate enough to see the elements in this formula firsthand when I recently spent the day in the Amputee Clinic on the Parkview Regional Medical Center (PRMC) campus.
Addressing a need
A few years ago, a local prosthetics vendor asked a Parkview Neurosciences physician, why there wasn’t an amputee clinic available to patients in the Fort Wayne area. With the need identified, the team went to work, and the Parkview Amputee Clinic opened in August 2022 on the lower level of Building 11 at PRMC.
With a full year under its belt, the clinic is held on the first and fourth Tuesday of each month, as one of five Neuroscience Multispecialty Clinics offered in the space. As the newest, the Amputee Clinic is still growing in comparison to the others, which include the Fall Prevention Clinic, Post-COVID Clinic, ALS Clinic and Interventional Movement Disorder Clinic.
I was greeted by Rhonda Ruch, the clinical coordinator for all of the Neuroscience Multispecialty Clinics. “We have a small clinic today,” she said. They were expecting three patients, a combination of recent amputees and some with new needs.
While there’s some overlap, each Neuroscience Multispecialty Clinic has a different care team. The Amputee Clinic is unique in that it’s the only offering run by PPG – Physical Medicine & Rehabilitation (PM&R) providers, a specialty of Parkview Neurosciences, led by Kyle Littell, MD. The physiatrist joined Parkview in September and, while he’s typically in the clinic, on the day of my shadow, he stayed at Parkview Hospital Randallia to oversee patient care in preparation for some time out of town. This allowed me to follow Kelsey Landis, NP, the other key clinician for the PM&R team.
Kelsey has been seeing patients in the Amputee Clinic since October 2023 and plays a key role in the referral process. “I do my best to see them following their surgery,” she said. “Our goal is to get them into the Amputee Clinic right away so we can support them through the whole journey.”
Comprehensive conversations
Each patient in the Amputee Clinic has access to a multidisciplinary team of experts, including Dr. Littell and Kelsey, physical therapists, an occupational therapist and prosthetic vendors.
Kelsey prepared for the first two patients of the afternoon, pulling up their charts to review their medical story, including surgical history, medications, and any prior or existing concerns.

The most common reasons for amputation include biomechanical issues, such as a bad ankle with unsuccessful repair, peripheral vascular complications (caused by a condition that results in a narrowing of the blood vessels), trauma, or, most commonly, infection. “We see this a lot with diabetic patients from unhealed wounds or patients who’ve had a joint replacement,” Kelsey explained. “Infections just tend to find and settle in those areas.” As she told a patient later that afternoon, “It’s so difficult to know when to decide to amputate. You keep thinking, maybe one more round of antibiotics will do it. But then you have to worry about damage to your kidneys from prolonged use of the medication. It’s incredibly hard.”
Individuals are asked to complete screening paperwork before their visit, which assesses stress and risk of depression, as well as any barriers that could be addressed through physical or occupational therapy.
Once she’s in with the patient, Kelsey tunes into the unique needs and tribulations of the individual. She begins her thorough evaluation with the skin. Are there any spots giving them trouble? Sores? Blisters? Wounds that won’t seem to heal? Friction is the enemy of the skin, and for amputees, friction can come from anywhere–a bunching sock at the top of the prosthetic, an ill-fitting component. She carefully runs her fingers along their scars, pausing if she detects a spot in need of attention. Throughout my shift in the clinic, I learned that in most instances, the limb needs touch. In the case of a tough area working through the healing process, Kelsey recommends massage.
She moves on to pain, a common foe for this population. Amputees often encounter pain from a variety of sources, including the nerves, muscles and bones. All three patients we saw reported phantom pain, a phenomenon in which individuals feel discomfort, such as itching or pain, in a part of the body that’s no longer there. “I don’t know how to express what I’m experiencing,” one amputee said.
This is a more troublesome close cousin to phantom sensation, which is the term for impulses to address a need for or move an extremity that has been amputated. Some might think they feel a tickle or try to wiggle their toes in a limb that is no longer there.
Kelsey works with the patient’s full care team, including their primary care provider and other specialists, to ensure any discomfort is being addressed while also being mindful of their list of medications and additional measures already prescribed. Due to the comorbidities of the patient population, as well as their symptoms, she and Dr. Littell often work in tandem with specialties like Podiatry, Wound Care, Endocrinology, Orthopedics, Emergency Medicine, Pain Management and Primary Care, always thoughtful about their role in the complex treatment puzzle.
She moves on to questions about the patient’s daily life. What does your home look like? Are there steps? Ramps? Are you working? How long is a shift? Do you have to lift or carry things? She combs through the logistics so she can understand the functionality they need routinely.
She ends by discussing their quality of life. And while this was the final inquiry of each team member who visited the patients, it was also the topic each was most passionate about. This is the product of their efforts, after all. Kelsey asks them about the things they love to do or want to get back to. She wanted to understand their hobbies, passions and people who light them up. “I have a two-year-old,” the first patient shared. “I need to be able to keep up with her.” Another gentleman disclosed that he played the drums before his surgery.
Kelsey considers all of these factors – the patient’s current abilities, willingness to work with therapy, personal and professional circumstances, and mindset – when developing the care plan and proper prosthetic for each patient. She evaluates their compliance with the care plan and estimates the effort needed for success. These pieces go into the prescription used to guide next steps.
Optimizing movement
When I met Cameron Buzzard, PT, the first thing that registered was his passion for his work. “The main goal of physical therapy is to address life barriers and set patients up for the best results with their prosthetic,” he explained.
And this should start earlier than people might think. “The quicker we can get these patients into PT, the better because that educational component is so important. We can see them within a few weeks of their procedure which allows us to set them up for success and prevent issues down the road.”
One example Cam shared was leg alignment. “After an amputation, while the patient is waiting for their prosthetic, it’s important they don’t just sit in their wheelchair. We want them to do things like lying on their stomach, so their hip flexors don’t get too tight, strengthening their glute muscles and managing their swelling. Having that guidance helps ensure that their prosthetic, not only fits when they get it, but that they’re strong enough and have proper alignment to get moving. Ideally, after a short time, someone should be able to put on their prosthetic and walk well.”
As he explained, the sooner a patient begins PT, the shorter their therapy journey will be. “We know that, in the midst of so much going on, people don’t want to think about the mechanics of alignment or leg position. But it is so important, and we can help them understand these concepts and get optimal results."
While discussing phantom pain, we were joined by Rachel Timmer, PTA, who others on the team credit with popularizing the phrase, “Show the limb some love.” If the prosthetic itself isn’t causing discomfort, it can be challenging to find a good solution for these patients. While the PT team might recommend things like compression or using a shrinker (an elastic sock used to control swelling) or more time in the socket (the connecting piece between the limb and prosthetic), Rachel strongly advocates stimulating the area. “It needs input,” she said. “Rubbing, massaging and brushing can expose the limb to new sensations and give feedback to the nerves.” These methods in combination with medicinal pain management strategies can help, but it’s difficult to provide complete relief for this frustrating symptom.
When the PT group, which included student Katie McClure, meets with patients, they create a comfortable environment, sitting at eye level, easing into questions about their activities and movement. They have the patient walk and assess their gait from all angles. “What we don’t want,” Cam explained, “is something like swinging the leg or compensating in some way that could eventually lead to hip or back issues.”
The team can identify needs like prosthetic adjustments – is it too high or too tight – and request referrals for additional therapies that might be beneficial to address things like balance, muscle weakness and wound healing challenges, if they haven’t already been identified by the clinician. “Skincare is so important,” Rachel said. “We see a lot of lymphedema and blisters with our amputees, so we stay on top of that.”

Amputee Clinic patients also have access to occupational therapy, though Jenn Ferguson, OT, was out on the day of my visit. “Jen is great about addressing any obstacles in the home, such as where grab bars would be helpful and modifications to make the day-to-day easier,” Rachel explained. One patient pointed out something as simple as catching his shoe on the underside ledge of his cabinets, which contributed to falls.
The North Star is getting patients back to the activities that bring them joy. “It breaks my heart I can’t walk my dog anymore,” one patient shared. Whether the aspiration is a stroll with a four-legged pal, house renovations, gardening, chasing a toddler, boxing or just making it through the grocery store, every member of the team in the Amputee Clinic listened and kept those dreams as the priority in their recommendations.
Amputee patients don’t have to use Parkview for physical and occupational therapy, but if they choose, Cam and Rachel hold sessions at Randallia. “You can go anywhere for therapy,” Cam said. “But I do recommend finding someone who is familiar and comfortable with amputee patients. It makes a big difference.”
Another differentiator in outcomes is a matter of personal effort. “If there’s something a patient wants to do, there’s typically a way to do it with their prosthetic, it’s just a matter of how,” Cam said. “We make sure they are comfortable and able to navigate things like stairs and daily activities, but success often hinges on their work between appointments. Someone who is putting in the time outside of their therapy sessions, which are typically one hour, twice a week, is going to be more successful than someone who isn’t.”
He shared that the most incredible aspect for him is watching the progress. “When I see someone the first visit and they’re in a wheelchair, and then the last visit they don’t need anything, it’s so rewarding,” he said. “Patients spend so much time with their therapists, so we truly connect on a personal level.”
Building a beneficial partnership
Vendors are an integral part of the comprehensive team at the Amputee Clinic. Representatives from SRT Prosthetics & Orthotics and Summit City Prosthetics & Orthotics attend the appointments to meet with patients who are already established with their products or just beginning the process of getting their custom-built prosthetic.
“Our patients can use any prosthetic vendor they want,” Kelsey explained. “We offer them literature that lists out all of their options. Their insurance is also a factor, of course, but it’s incredibly beneficial having them on-site to answer questions and meet with the patients.”
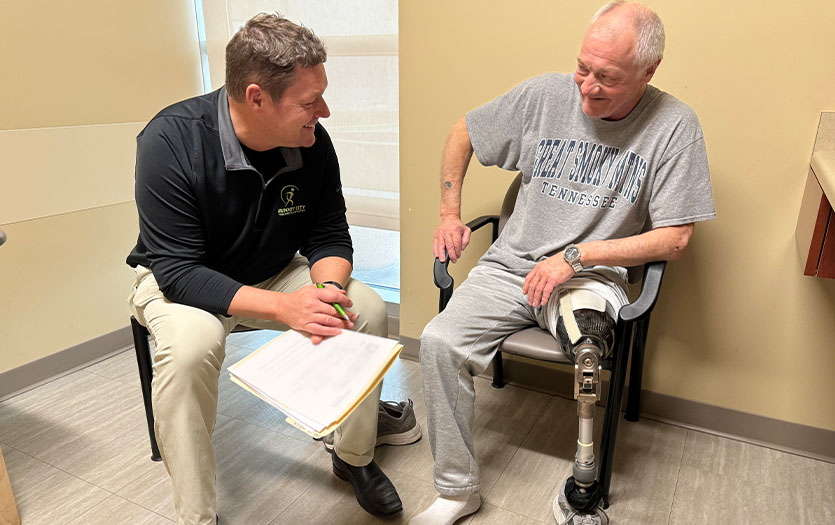
After Kelsey and I left one patient’s room, Jason Timmer from Summit City went in for a consultation. “I built his leg for him,” he shared after their time together. This surprised me, as I’d assumed these representatives were in roles similar to sales. But quite the contrary. Jason and the representative with SRT are hands-on in the prosthetics process, from casting or gathering 3D digitally scanned images of the limb to forming the components the patient will wear daily.
Countless factors play into the creation of a prosthetic. With feedback from the individual, clinical team and therapists, the manufacturer also has to consider things like weight management. If a patient has been immobile and plans to increase activity, it can lead to weight loss and ultimately how the prosthetic fits. The same is true in the other direction if their movement declines and they put on weight.
They also consider things like the terrain the person will encounter frequently. Is it even? Do they need to propel? What is the level at which they need to function? Prosthetics are ranked based on mobility level, from K-1 for less mobile individuals to K-4, prosthetics designed for the most active amputees. “We want to get the prosthetic that works for their life,” Jason said.

Each prosthetic consists of four components. The socket (where the limb is held), appendage (the hand or foot), joint (the moveable aspect akin to a wrist, elbow, shoulder, ankle, knee or hip) and the connecting module, which attaches the appendage and joint to the socket. Next, the manufacturer, patient and care team have to evaluate the best suspension system for the individual and their needs. This is the mechanism for attaching and keeping all of the components in place.
For all of the details that go into creating a prosthetic, I was perhaps most blown away by the sophistication. Today’s prosthetics can offer biofeedback data and utilize smart technology. “You’re getting a microprocessor and a new socket,” Jason told one patient, as I observed nearby. “You’ll have a computerized knee that can think for you. It will respond to how you bend, your balance, how your weight shifts.” The patient’s face showed what I was thinking. Science and technology are incredible. Jason gathered some basic intel – height, weight, shoe size, activities – and began the process. Once authorized, creating the prosthetic goes fairly quickly.
But Jason wasn’t just focused on the new. He also assessed the patient’s current prosthetic, asking about falls and pain. He investigated which sock ply the gentleman was using (they come in 1-, 3- or 5-ply options), what was tight and what was loose. While Jason didn’t have his tools that particular day, patients are always welcome to meet him at his office for adjustments.
Jason recommended PT and inquired about muscle spasms, and any rubbing or pressure, which can lead to problematic wounds. They chatted briefly about the weight of the prosthetic and if it felt comfortable. In all aspects of his conversation with the patient, as with PT and Kelsey, the focus was on optimizing the person’s current circumstances, mitigating potential risks and adding quality to their days.
Before he left, Jason asked, “How else can I help improve your life?”
The big wins
While some of the benefits of the Amputee Clinic are obvious, such as access to vendors, specialized PM&R clinicians, and physical and occupational therapists, in one office, some are less familiar.
For both new and prior amputees, being established as a patient in the Amputee Clinic can expedite the process throughout the journey. “Speed and timing are huge benefits for patients,” Cam said. “People don’t always realize everything that goes on behind the scenes–the paperwork, signatures, routing. Here, patients can take care of everything at the same time. The provider is here. The vendor is here. The therapists are here. We can communicate, collaborate and get paperwork processed much faster.”
This also extends to supplies. “For a lot of our patients, insurance will cover yearly consumables,” Rachel said. “It’s much easier to get those prescriptions if you’re established. It streamlines the annual process.”
In addition to access to specialized care, supplies and adjustments, one of the most significant shifts for patients who attend the Amputee Clinic is that of a longevity mindset. They aren’t given a prosthetic and then released to find their way on their own. They have a team around them from the post-op stage through their years of maintenance, including any improvements or upgrades they could benefit from as their circumstances and the technology evolve. “Being in a cadence keeps communication open,” Kelsey said. “And it helps us stay in front of any potential complications, so the patient can really have healthier, happier outcomes.”
With the right team, the will to do the work, a gracious attitude, healthy curiosity and that seedling of hope, the sky’s the limit for the patients in the Amputee Clinic.
The clinic encourages patients to work with their primary care provider, Parkview or otherwise, to acquire a referral. They can then connect with the individual for a brief screening to make sure that the clinic is an appropriate fit. “Most amputees, no matter what stage they’re in, are great candidates for the clinic,” Kelsey said. “Once their stitches or staples are out, usually four to six weeks post-op, we can get them on the schedule. The important thing is that their wound is completely healed.” Most patients are seen every 12 weeks or so for follow-up, though this changes based on their needs as they grow more comfortable in their prosthetic.
Between scheduled appointments, the specialized team in the Amputee Clinic is always available to their patients and willing to assist with any complications or questions. The number of providers will expand this fall, as the first cohort of PM&R residents join Dr. Littell as part of their rotation. It’s just one more way Parkview is educating the clinicians of tomorrow while supporting the patients we serve.
For more information or to schedule an appointment, call 260-425-6780 or visit parkview.com/AmputeeClinic.



